Orthopaedics In Action Fracture Repair Worksheet Answers
Onlines
Mar 10, 2025 · 8 min read
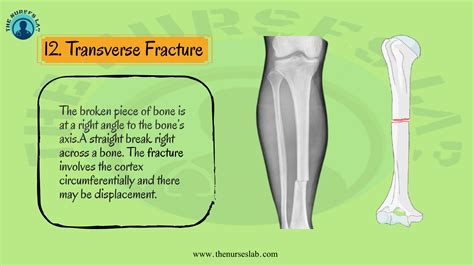
Table of Contents
Orthopaedics in Action: Fracture Repair Worksheet Answers & Comprehensive Guide
This comprehensive guide delves into the intricacies of fracture repair, providing detailed answers to common worksheet questions encountered in orthopaedics courses and offering a broader understanding of the subject. We will explore various fracture types, treatment methods, and the critical considerations involved in successful fracture management. This resource aims to be a valuable tool for students, professionals, and anyone interested in learning more about this vital area of orthopaedics.
Understanding Fracture Classification
Before delving into specific repair techniques, a solid grasp of fracture classification is essential. Several systems exist, but the most common involves considering the following factors:
1. Anatomic Location: This specifies the bone affected (e.g., femur, tibia, humerus) and the precise location of the fracture within that bone (e.g., midshaft, distal, proximal).
2. Fracture Pattern: This describes the nature of the break:
- Transverse: A fracture line perpendicular to the long axis of the bone.
- Oblique: A fracture line at an angle to the long axis of the bone.
- Spiral: A fracture line that spirals around the bone, often resulting from a twisting force.
- Comminuted: A fracture with multiple fragments of bone.
- Segmental: A fracture with two or more fracture lines, resulting in a segment of bone isolated between fractures.
- Avulsion: A fracture caused by a tendon or ligament pulling off a piece of bone.
- Impacted: A fracture where one bone fragment is driven into another.
- Greenstick: An incomplete fracture, common in children, where one side of the bone bends while the other fractures.
3. Displacement: This refers to the relationship between the fractured bone ends:
- Non-displaced: The bone ends are aligned.
- Displaced: The bone ends are not aligned. This may involve angulation (bending), shortening, or rotation.
4. Open vs. Closed: This distinguishes between fractures where the bone breaks through the skin (open or compound fracture) and those where the skin remains intact (closed fracture). Open fractures carry a significantly higher risk of infection.
Fracture Repair Techniques: A Detailed Overview
Numerous techniques exist for repairing fractures, each selected based on the specific characteristics of the fracture and the patient's overall health.
1. Closed Reduction: This non-surgical approach involves manually manipulating the fractured bone fragments into alignment. It's often used for non-displaced or minimally displaced fractures. Immobilization with a cast, splint, or external fixator is usually necessary to maintain alignment and promote healing.
2. Open Reduction and Internal Fixation (ORIF): This surgical technique involves surgically exposing the fracture site, aligning the bone fragments, and then stabilizing them with internal fixation devices such as plates, screws, rods, or wires. ORIF is often necessary for displaced fractures, comminuted fractures, or fractures that are unstable after closed reduction.
3. External Fixation: This technique involves using pins or screws inserted through the skin and into the bone fragments, connected to an external frame. It's useful for complex fractures, particularly those with significant soft tissue damage, or situations where internal fixation is not feasible. External fixation allows for easier wound care and monitoring but is associated with some risks, including pin-site infections.
4. Intramedullary Nailing: This involves inserting a long rod (nail) into the medullary canal (the hollow center) of the bone to stabilize the fracture. This is a common technique for long bone fractures such as femoral and tibial fractures. It offers good stability and allows for early mobilization.
Worksheet Answer Examples & Explanations
Let's address potential questions from an Orthopaedics in Action fracture repair worksheet:
Question 1: Describe the difference between a transverse and an oblique fracture. Provide examples of mechanisms of injury for each.
Answer: A transverse fracture has a fracture line perpendicular to the long axis of the bone. This typically results from a direct blow perpendicular to the bone. For example, a direct fall onto the outstretched arm could cause a transverse fracture of the radius or ulna. An oblique fracture has a fracture line at an angle to the long axis of the bone. This often results from a twisting force or a combination of direct and indirect forces. A spiral fracture, a subtype of oblique fracture, frequently results from a twisting injury, such as a skiing accident.
Question 2: Explain the importance of proper fracture reduction and immobilization.
Answer: Proper fracture reduction (restoring anatomical alignment) is crucial for optimal healing and functional recovery. Misalignment can lead to malunion (healing in a deformed position), non-union (failure to heal), and long-term complications. Immobilization, using casts, splints, external fixators, or internal fixation devices, is essential to maintain the reduced position and prevent further displacement, thereby promoting healing and minimizing complications.
Question 3: Compare and contrast open reduction internal fixation (ORIF) and external fixation.
Answer: Both ORIF and external fixation are surgical methods used to treat fractures. ORIF involves surgically exposing the fracture, aligning the bone fragments, and then using internal devices (plates, screws, etc.) for stabilization. It offers excellent stability and generally results in better alignment. However, it requires a more invasive surgery with a higher risk of infection and complications. External fixation uses pins inserted through the skin and into the bone fragments, connected to an external frame. It's less invasive than ORIF and is particularly useful for fractures with significant soft tissue damage. However, it is less stable and may be associated with pin-site infections and potential complications related to the external frame. The choice depends on the specific fracture characteristics and patient factors.
Question 4: What are some potential complications associated with fracture healing?
Answer: Several complications can occur during fracture healing. These include:
- Nonunion: Failure of the fracture to heal completely.
- Malunion: Healing in a deformed position.
- Delayed union: Slower than expected healing.
- Infection: Particularly common in open fractures.
- Compartment syndrome: A serious condition involving increased pressure within a muscle compartment, potentially leading to tissue damage.
- Nerve or vessel injury: Damage to nearby nerves or blood vessels.
- Osteonecrosis (avascular necrosis): Bone death due to disruption of blood supply.
- Complex Regional Pain Syndrome (CRPS): A chronic pain condition that can develop after an injury.
Question 5: Discuss the role of imaging in fracture management.
Answer: Imaging plays a critical role in fracture management, from initial diagnosis to monitoring healing. X-rays are the primary imaging modality used to identify fractures, assess displacement, and evaluate healing. Other imaging techniques, such as CT scans and MRI scans, may be used to provide more detailed information, particularly in complex fractures or when assessing soft tissue damage. Imaging helps guide treatment decisions, monitor the effectiveness of treatment, and identify potential complications.
Question 6: Describe the principles of fracture healing.
Answer: Fracture healing is a complex biological process involving several stages:
- Inflammation: Immediately after the fracture, inflammation occurs, characterized by bleeding, swelling, and pain. This stage is crucial for initiating the healing cascade.
- Soft Callus Formation: Within days to weeks, a soft callus forms, consisting of fibrous tissue and cartilage. This soft callus bridges the fracture gap.
- Hard Callus Formation: Over several weeks, the soft callus is gradually replaced by a hard callus, composed of woven bone. This provides increasing stability to the fracture.
- Remodeling: The final stage involves the gradual remodeling of the hard callus into mature lamellar bone, restoring the original bone architecture. This can take months or even years depending on the fracture type and location.
Beyond the Worksheet: Advanced Considerations in Fracture Repair
This section explores more nuanced aspects of fracture repair, expanding on the foundational knowledge provided earlier.
Factors Influencing Fracture Healing
Numerous factors can influence fracture healing, including:
- Patient age and overall health: Older patients and those with underlying medical conditions (diabetes, osteoporosis) may experience slower healing.
- Fracture characteristics: The type, location, and displacement of the fracture affect healing time. Comminuted and displaced fractures typically heal slower.
- Soft tissue damage: Significant soft tissue injury can impair blood supply and hinder healing.
- Infection: Infection dramatically slows healing and can lead to nonunion.
- Smoking: Nicotine reduces blood flow and negatively impacts healing.
- Nutrition: Adequate nutrition, especially sufficient calcium and vitamin D, is essential for bone healing.
- Immobilization: Inadequate immobilization can lead to delayed union or nonunion.
Advanced Fracture Repair Techniques
Beyond the techniques already discussed, several advanced techniques are employed in complex cases:
- Bone grafting: Used to fill bone defects or stimulate healing in nonunions.
- Bone stimulation: Techniques like electrical stimulation or ultrasound are sometimes used to promote healing.
- Distraction osteogenesis: A technique involving gradual distraction (lengthening) of the bone to treat bone defects or limb lengthening.
Rehabilitation after Fracture Repair
Rehabilitation is a critical component of fracture management. It aims to restore range of motion, strength, and function. The specific rehabilitation program depends on the fracture location, the repair technique used, and the patient's individual needs. It may involve physical therapy, occupational therapy, and other interventions.
This comprehensive guide provides a thorough overview of orthopaedics in action, specifically focusing on fracture repair. It aims to clarify many common questions, providing detailed answers and expanding on the fundamental concepts. Remember, this information is for educational purposes only and should not be substituted for professional medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Latest Posts
Latest Posts
-
Unit Chemical Bonding Covalent Bonding Ws 3
Mar 10, 2025
-
Gizmos Student Exploration Adding Vectors Answer Key
Mar 10, 2025
-
Unit 9 Progress Check Mcq Ap Lang
Mar 10, 2025
-
Allow A Larger Space Cushion Than Usual When Stopping
Mar 10, 2025
-
An Automobile Manufacturer Sold 30000 New Cars
Mar 10, 2025
Related Post
Thank you for visiting our website which covers about Orthopaedics In Action Fracture Repair Worksheet Answers . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
