Part B Practice Interpreting Electrocardiograms Answers
Onlines
Mar 12, 2025 · 8 min read
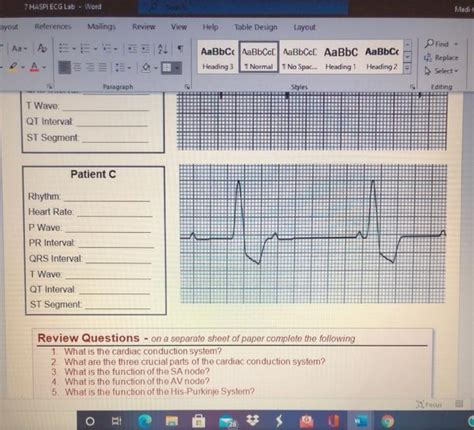
Table of Contents
Part B Practice Interpreting Electrocardiograms: Answers and Deep Dive
Mastering electrocardiogram (ECG) interpretation is crucial for healthcare professionals. This comprehensive guide delves into the answers for a hypothetical Part B ECG interpretation practice set, providing detailed explanations and linking them to underlying cardiac physiology. While specific ECG strips aren't provided here (as this is a text-based response), we'll cover common ECG findings and their interpretations to build your understanding. Remember, real-world ECG interpretation requires careful consideration of the entire clinical picture, including patient history and physical examination findings. This guide focuses solely on the ECG interpretation aspects.
Understanding the Basics: A Quick Review
Before diving into the answers, let's refresh some key ECG concepts. The ECG provides a graphical representation of the electrical activity of the heart. Key elements include:
- P wave: Represents atrial depolarization (contraction).
- QRS complex: Represents ventricular depolarization (contraction).
- T wave: Represents ventricular repolarization (relaxation).
- PR interval: Time from the start of atrial depolarization to the start of ventricular depolarization.
- QT interval: Time from the start of ventricular depolarization to the end of ventricular repolarization.
- ST segment: Represents the early phase of ventricular repolarization. Changes here often indicate ischemia or infarction.
Hypothetical Part B ECG Scenarios and Interpretations
This section outlines potential scenarios from a Part B ECG practice exam and provides detailed answers, focusing on the key ECG features and their clinical significance. Remember, this is a simulated practice; always consult with experienced professionals for real-life cases.
Scenario 1: Sinus Bradycardia
ECG Findings: Regular rhythm; heart rate <60 bpm; normal P waves preceding each QRS complex; normal PR interval; normal QRS duration.
Interpretation: Sinus bradycardia is a slow heart rate originating from the sinoatrial (SA) node. This can be normal in athletes or during sleep but may indicate underlying pathology like hypothyroidism, increased vagal tone, or myocardial infarction in other contexts. Treatment depends on the patient's symptoms; symptomatic bradycardia may require pacing.
Key Considerations: While a slow heart rate is the defining feature, assess the overall rhythm regularity and the presence of any other abnormalities. Absence of other abnormalities suggests a benign origin, while presence of other issues points to underlying pathology.
Scenario 2: Sinus Tachycardia
ECG Findings: Regular rhythm; heart rate >100 bpm; normal P waves preceding each QRS complex; normal PR interval; normal QRS duration.
Interpretation: Sinus tachycardia is a rapid heart rate originating from the SA node. Causes include physiological stress (exercise, anxiety, fever), dehydration, hypovolemia, anemia, hyperthyroidism, and various cardiac conditions. Management focuses on treating the underlying cause.
Key Considerations: Differentiate between sinus tachycardia and other tachyarrhythmias like atrial flutter or fibrillation. The regularity of the rhythm and presence of normal P waves are crucial differentiating features. Observe the patient’s clinical presentation as well – tachycardia can be normal in response to certain physiological demands.
Scenario 3: Atrial Fibrillation
ECG Findings: Irregularly irregular rhythm; absent P waves; fibrillatory waves (f waves); variable R-R intervals; normal QRS duration (unless underlying conduction abnormalities present).
Interpretation: Atrial fibrillation (AFib) is a common arrhythmia characterized by chaotic atrial activity. This leads to an irregularly irregular rhythm and loss of the distinct P waves. Risk factors include hypertension, heart failure, valvular heart disease, and aging. Management focuses on rate control, rhythm control, and stroke prevention (anticoagulation).
Key Considerations: AFib is a significant clinical problem. It may manifest as palpitations, shortness of breath, or chest pain. The clinical presentation and potential for thromboembolic events necessitate prompt evaluation and management.
Scenario 4: Atrial Flutter
ECG Findings: Regular or irregularly irregular rhythm; sawtooth pattern of flutter waves (F waves); characteristic flutter waves replacing the P waves; the atrial rate typically ranges from 250 to 350 beats per minute; ventricular response varies depending on AV node conduction.
Interpretation: Atrial flutter represents another atrial arrhythmia with a rapid atrial rate. The characteristic sawtooth pattern of flutter waves helps differentiate it from AFib. Management involves rate control and rhythm control, sometimes requiring catheter ablation.
Key Considerations: While atrial flutter often presents similarly to AFib, the distinct sawtooth pattern is crucial for diagnosis. Understanding the ratio of atrial to ventricular rates is crucial for interpreting the severity and potential implications.
Scenario 5: Ventricular Tachycardia
ECG Findings: Rapid heart rate (usually >100 bpm); wide QRS complexes (>0.12 seconds); absence of P waves; typically irregular rhythm.
Interpretation: Ventricular tachycardia (VT) is a life-threatening arrhythmia characterized by rapid ventricular depolarizations originating from a site other than the SA node. It can be sustained or non-sustained, and its implications depend on the patient's hemodynamic status. Treatment involves immediate cardioversion or defibrillation in hemodynamically unstable patients and antiarrhythmic medications in stable patients.
Key Considerations: VT represents a significant clinical emergency. Immediate recognition and appropriate intervention are critical for improving patient outcomes. Identifying the QRS morphology and distinguishing VT from supraventricular tachycardias with aberrant conduction is crucial.
Scenario 6: Premature Ventricular Contractions (PVCs)
ECG Findings: Premature beats; wide and bizarre QRS complexes; often followed by a compensatory pause.
Interpretation: PVCs are premature beats originating from the ventricles. They are commonly observed and may be benign in healthy individuals, but in some cases, they can indicate underlying myocardial damage or electrolyte imbalances. Management depends on the frequency, morphology, and patient's overall cardiac status.
Key Considerations: The clinical significance of PVCs varies. Infrequent PVCs might be benign, but frequent or complex PVCs might necessitate further investigation and potentially treatment, including addressing underlying causes like electrolyte abnormalities or ischemia. The presence of multifocal PVCs may indicate a more significant underlying issue.
Scenario 7: Left Bundle Branch Block (LBBB)
ECG Findings: Wide QRS complexes (>0.12 seconds); notched R waves in the left precordial leads (V5, V6); deep S waves in the right precordial leads (V1, V2); ST-segment and T-wave changes are often present, usually discordant with the QRS complex.
Interpretation: LBBB represents a delay or block in the conduction of the electrical impulse through the left bundle branch. It's often associated with underlying structural heart disease such as coronary artery disease, hypertension, or valvular heart disease. Management involves addressing the underlying cause.
Key Considerations: Differentiating LBBB from other wide QRS complex tachyarrhythmias is vital. LBBB can be a benign finding, but in the context of chest pain or other symptoms, it raises concerns for myocardial ischemia or infarction. It's imperative to look for accompanying signs of ischemia or infarction.
Scenario 8: Right Bundle Branch Block (RBBB)
ECG Findings: Wide QRS complexes (>0.12 seconds); RSr' pattern in the right precordial leads (V1, V2); slurred S waves in the left precordial leads (V5, V6).
Interpretation: RBBB indicates a delay or block in the conduction of the electrical impulse through the right bundle branch. It may be benign or associated with underlying structural heart disease, such as pulmonary hypertension or cor pulmonale. Management depends on the underlying cause and the patient's symptoms.
Key Considerations: RBBB often has a less significant impact than LBBB. However, its presence in the context of acute coronary syndromes may signal posterior myocardial infarction. Always carefully assess the entire ECG tracing and correlate it with the clinical presentation.
Scenario 9: ST-segment Elevation Myocardial Infarction (STEMI)
ECG Findings: ST-segment elevation in two or more contiguous leads; reciprocal ST-segment depression may be present; often associated with T-wave inversions or hyperacute T waves in the early stages of infarction.
Interpretation: STEMI indicates a complete occlusion of a coronary artery, leading to myocardial necrosis. This is a life-threatening emergency requiring immediate intervention with reperfusion therapy (e.g., percutaneous coronary intervention or thrombolytic therapy).
Key Considerations: STEMI requires prompt recognition and treatment. The location of the ST-segment elevation helps pinpoint the affected coronary artery and the area of the heart involved. Delay in treatment can lead to significant morbidity and mortality.
Scenario 10: ST-segment Depression Myocardial Ischemia
ECG Findings: ST-segment depression; T-wave inversion. These findings may be subtle or nonspecific, and they often occur in multiple leads.
Interpretation: ST-segment depression typically signifies myocardial ischemia (reduced blood flow to the heart muscle). The findings are often less dramatic than STEMI. It frequently indicates unstable angina pectoris. Management involves careful evaluation for acute coronary syndrome.
Key Considerations: ST-segment depression can be a subtle sign, making accurate interpretation crucial. It needs to be correlated with the patient's symptoms, such as chest pain, shortness of breath, or diaphoresis. Further investigations, such as cardiac enzymes and coronary angiography, are often needed to confirm the diagnosis.
Beyond the Basics: Advanced ECG Interpretation
Mastering ECG interpretation requires more than just recognizing basic rhythms. It involves understanding:
- Axis Deviation: Determining the overall direction of electrical conduction through the heart.
- Hypertrophy: Recognizing signs of enlarged chambers (e.g., left ventricular hypertrophy).
- Electrolyte Imbalances: Identifying ECG changes associated with conditions like hypokalemia and hyperkalemia.
- Drug Effects: Understanding how certain medications can alter ECG findings.
Practical Tips for ECG Interpretation
- Systematic Approach: Develop a consistent approach to ECG interpretation, checking for rate, rhythm, P waves, QRS complexes, intervals, and ST segments.
- Clinical Correlation: Always correlate ECG findings with the patient's clinical presentation, history, and physical examination.
- Practice, Practice, Practice: Regular practice is essential for developing expertise in ECG interpretation. Use online resources, textbooks, and simulated cases to hone your skills.
- Seek Mentorship: Work with experienced clinicians to learn from their expertise and gain valuable feedback on your interpretations.
Conclusion
ECG interpretation is a vital skill for healthcare professionals. While this guide provides answers to hypothetical Part B ECG practice scenarios and detailed explanations, remember that real-world application requires experience, clinical judgment, and a comprehensive understanding of cardiac physiology. Continuous learning, regular practice, and seeking guidance from experts are crucial to developing proficiency in this critical skill. Always prioritize patient safety and consult with senior clinicians when facing challenging or uncertain situations. This information is for educational purposes and should not be considered a substitute for professional medical advice.
Latest Posts
Latest Posts
-
For Which Of The Following Is Potential Energy Increasing
Mar 12, 2025
-
Chapter Summaries Of The Great Gatsby
Mar 12, 2025
-
If Alicia Wants To Consider Making A Change
Mar 12, 2025
-
The Left Hand Of Darkness Summary By Chapter
Mar 12, 2025
-
Suppose You Are Walking Down A Street
Mar 12, 2025
Related Post
Thank you for visiting our website which covers about Part B Practice Interpreting Electrocardiograms Answers . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
