Single-payer Systems Typically Apply All Of The Following Practices Except:
Onlines
Mar 09, 2025 · 6 min read
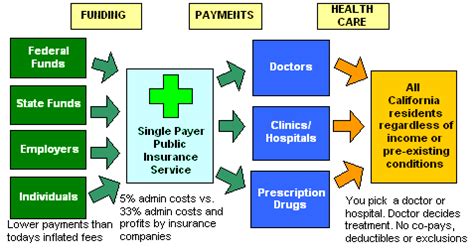
Table of Contents
Single-Payer Healthcare: Deconstructing the Myths and Unveiling the Realities
Single-payer healthcare systems, often a subject of intense debate, represent a model where a single public entity, typically the government, funds healthcare services for all citizens. While proponents champion its potential for universal coverage and cost control, critics raise concerns about efficiency, choice, and potential government overreach. Understanding the core operational principles of such systems is crucial for informed discussion. This article delves into the common practices employed in single-payer models, highlighting what they typically do not include.
Before we delve into the specifics, it's essential to clarify that "single-payer" doesn't dictate a single delivery model. The funding mechanism is centralized, but the provision of care can involve a mixed landscape of public and private providers. This distinction is vital for accurately assessing the system's characteristics.
Common Practices in Single-Payer Systems
Several practices are frequently observed in single-payer healthcare systems globally. These include:
-
Universal Coverage: The defining feature is the provision of healthcare services to all citizens, regardless of their ability to pay. This eliminates the financial barrier to essential medical care, a significant advantage for many.
-
Negotiated Rates: Single-payer systems often negotiate prices directly with healthcare providers, creating leverage to control costs. This differs significantly from the fee-for-service model prevalent in some other systems, which can lead to inflated prices driven by market forces. This negotiation power aims to balance affordability with the need to maintain a robust healthcare infrastructure.
-
Emphasis on Primary Care: Many single-payer systems prioritize primary care, aiming to prevent illnesses through early detection and management. This proactive approach can lead to better health outcomes in the long run and reduce the need for expensive specialized care later on.
-
Regulation of Healthcare Services: These systems generally involve significant government regulation over the healthcare sector. This regulation can encompass various aspects, from licensing of providers to determining which services are covered under the system. This regulatory oversight is crucial for maintaining quality standards and ensuring equitable access.
-
Focus on Public Health Initiatives: A strengthened public health infrastructure is often a hallmark of single-payer systems. This includes initiatives focused on preventative care, disease control, and health education, all contributing to a healthier population.
-
Centralized Administration: The centralized funding and administrative structure often leads to a more streamlined system, potentially reducing administrative overhead compared to systems with multiple insurers. However, the level of centralization and efficiency can vary widely depending on the specific implementation.
What Single-Payer Systems Typically Do Not Apply:
While the above practices are common, it's crucial to understand what single-payer systems generally do not encompass:
1. Unfettered Choice of Providers: While most single-payer systems aim for broad access, they rarely offer completely unrestricted choice of provider. There are often limitations based on factors such as geographic location, provider network participation, and specific service availability. This doesn't necessarily translate to a lack of choice; rather, it's a controlled approach to managing resources and ensuring quality standards across participating providers.
2. Complete Absence of Private Insurance: The term "single-payer" doesn't automatically equate to the complete elimination of private insurance. Many single-payer systems allow for supplemental private insurance to cover services not included in the basic plan or to provide access to amenities beyond what is publicly funded. This supplemental coverage often addresses aspects such as faster access to specialist care or private hospital rooms.
3. Unrestricted Patient Choice of Treatment: While patients generally have a broad range of treatment options covered, single-payer systems often implement guidelines and protocols to ensure cost-effectiveness and appropriate use of resources. This can involve clinical pathways or prior authorization procedures for specific treatments or procedures. The goal here isn't necessarily to restrict access to needed care, but rather to promote efficient use of resources and minimize unnecessary or ineffective procedures.
4. Completely Eliminated Waiting Lists: Although single-payer systems aim to provide timely access to care, completely eliminating waiting lists is often a challenge, particularly for elective procedures or specialized services. The extent of waiting lists can vary widely depending on the specific system's capacity, resource allocation, and overall demand for services. Waiting times frequently become a point of contention in public discourse surrounding single-payer models.
5. Guaranteed Elimination of All Healthcare Costs: While the aim is to make healthcare affordable and accessible, single-payer systems usually do not cover all healthcare expenses. There might still be out-of-pocket costs for certain services, such as dental care, vision care, or prescription drugs, depending on the specific design of the system. These variations in coverage often fuel further public debate and scrutiny of system efficacy.
6. Immediate and Complete System Transformation: The transition to a single-payer system is rarely a swift process. It's often a gradual transition involving phased implementation, adaptation to existing infrastructure, and overcoming various logistical hurdles. Existing healthcare providers, institutions, and the workforce itself need time to adjust to the new paradigm.
Comparing and Contrasting Single-Payer Systems Globally
It is important to remember that single-payer systems, despite sharing core principles, differ significantly in their implementation across various countries. The Canadian system, for instance, differs considerably from the British National Health Service (NHS), reflecting unique historical contexts, healthcare infrastructure, and societal values. Analyzing these differences is crucial to understanding the nuances and complexities inherent in different models. Factors such as the extent of private sector involvement, the level of government regulation, and the emphasis on different aspects of healthcare delivery all contribute to the unique characteristics of each national system.
Addressing Common Criticisms of Single-Payer Systems
Single-payer systems are frequently criticized for potential drawbacks. Concerns are often raised about the potential for longer wait times, limited choice of providers, and the risk of government bureaucracy hindering efficiency. These concerns are not always unfounded, and their validity varies depending on the specific implementation of the system. However, proponents of single-payer systems often argue that these potential drawbacks are outweighed by the benefits of universal coverage and cost control, ultimately leading to improved population health outcomes.
Conclusion: A nuanced perspective
Single-payer healthcare systems present a complex tapestry of practices and challenges. While they aim for universal coverage, cost control, and equitable access, it's crucial to understand their limitations. The complete absence of private insurance, unfettered provider choice, the immediate eradication of waiting lists, or the total elimination of out-of-pocket costs are generally not characteristics of these systems. A thorough and nuanced understanding of their strengths and weaknesses is essential for informed debate and effective policy-making in this critical sector. The ongoing debate about single-payer models highlights the importance of ongoing evaluation and refinement to ensure the most efficient and equitable access to healthcare for all. Further research and comparative studies across various single-payer systems globally are crucial for optimizing these models and improving healthcare outcomes worldwide. The specific context and unique circumstances of each country need to be taken into account when assessing the effectiveness and applicability of single-payer models.
Latest Posts
Latest Posts
-
A Wrinkle In Time Summary By Chapter
Mar 09, 2025
-
Which Statement Best Describes The Purpose Of Combined Functional Teams
Mar 09, 2025
-
Logisctix Company Had The Following Tiems
Mar 09, 2025
-
Order The Words To Form Superlative Sentences
Mar 09, 2025
-
What Is Broadcast Address For 172 16 200 130 26
Mar 09, 2025
Related Post
Thank you for visiting our website which covers about Single-payer Systems Typically Apply All Of The Following Practices Except: . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
