Soap Note For Urinary Tract Infection
Onlines
Mar 26, 2025 · 7 min read
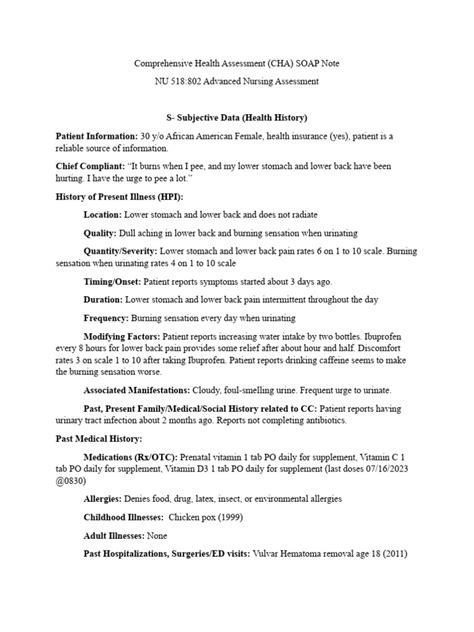
Table of Contents
SOAP Note for Urinary Tract Infection (UTI)
A Urinary Tract Infection (UTI) is a common bacterial infection affecting the urinary system. A well-structured SOAP note is crucial for documenting patient encounters, facilitating clear communication among healthcare providers, and ensuring optimal patient care. This comprehensive guide will delve into creating a thorough and accurate SOAP note for a patient presenting with a UTI.
Understanding the SOAP Note Format
The SOAP note follows a structured format, using the acronym SOAP to represent its components:
- S: Subjective – This section details the patient's self-reported symptoms and medical history. It’s what the patient tells you.
- O: Objective – This section encompasses the measurable and observable findings during the physical examination and diagnostic testing. It's what you observe and measure.
- A: Assessment – This section involves the clinical diagnosis based on the subjective and objective findings. It's your interpretation of the S and O.
- P: Plan – This section outlines the treatment plan, including medication, follow-up appointments, and patient education. It's what you will do.
Example SOAP Note for a UTI
Let's illustrate a complete SOAP note for a patient presenting with symptoms suggestive of a UTI.
Patient: Jane Doe, 35-year-old female
Date: October 26, 2024
S: Subjective
- Chief Complaint (CC): Burning on urination, frequent urination, urgency.
- History of Present Illness (HPI): Ms. Doe reports experiencing burning pain during urination (dysuria) for the past three days. She also notes increased urinary frequency (frequency) and a strong urge to urinate (urgency). She denies any fever, chills, flank pain, or hematuria (blood in the urine). She reports no known allergies. She states that she has experienced UTIs in the past, typically treated successfully with antibiotics.
- Past Medical History (PMH): Appendectomy at age 12. No other significant medical history.
- Past Surgical History (PSH): Appendectomy at age 12.
- Family History (FH): Mother has a history of hypertension. No family history of kidney stones or recurrent UTIs.
- Social History (SH): Ms. Doe denies smoking, illicit drug use, or excessive alcohol consumption. She reports drinking plenty of water throughout the day. She is sexually active with one partner. She denies any recent changes in sexual practices.
- Medications: None currently.
- Allergies: None known.
- Review of Systems (ROS): Generally negative except for genitourinary symptoms as described above. She denies any gastrointestinal, respiratory, cardiovascular, or neurological symptoms.
O: Objective
- Vital Signs: Temperature: 98.6°F (37°C); Pulse: 72 bpm; Respirations: 16 breaths/min; Blood Pressure: 120/80 mmHg.
- Physical Examination: General appearance is well-nourished and alert. Abdomen is soft, non-tender, and non-distended. Costovertebral angle (CVA) tenderness is absent bilaterally. Pelvic exam reveals no significant abnormalities.
- Laboratory Data:
- Urinalysis: Positive for leukocytes esterase, nitrites, and bacteria. Microscopic examination reveals numerous white blood cells and bacteria.
- Urine Culture: Pending (results to be obtained within 24-48 hours).
A: Assessment
- Diagnosis: Uncomplicated urinary tract infection (UTI), likely due to Escherichia coli (E. coli) based on the urinalysis results. The absence of fever, chills, and flank pain suggests it is an uncomplicated UTI.
P: Plan
- Treatment: Prescribe a 3-day course of trimethoprim-sulfamethoxazole (TMP-SMX) 160/800mg twice daily. Alternatively, consider nitrofurantoin 100mg twice daily for 5 days if the patient has any allergies to sulfa drugs. Instruct the patient on appropriate medication use, including completing the full course of antibiotics.
- Patient Education: Instruct Ms. Doe on increasing her fluid intake to help flush out bacteria. She should be encouraged to urinate frequently and avoid caffeine and alcohol, which can irritate the bladder. Advise her to avoid delaying urination. Emphasize the importance of completing the entire course of antibiotics even if symptoms improve. Inform her to return if her symptoms worsen or persist after finishing the antibiotic course. Discuss strategies to prevent recurrent UTIs, such as proper hygiene practices after urination and bowel movements.
- Follow-up: Schedule a follow-up appointment in one week to assess the response to treatment and obtain the urine culture results. The culture results will confirm the causative organism and ensure appropriate antibiotic coverage. If symptoms persist, further investigation will be considered.
Expanding on Key Sections for Improved SEO and Readability
Let’s expand on several key sections to enhance the SEO and overall readability of the SOAP note description. This will incorporate relevant keywords naturally and improve semantic understanding.
Subjective: Deeper Dive into Symptoms and History
The subjective section can be enriched by including more detail on symptom characteristics. For example:
-
Dysuria Specificity: Instead of simply "burning on urination," specify the severity ("severe burning," "mild burning"), timing ("burning at the beginning," "burning at the end," "constant burning"), and any associated symptoms (e.g., "accompanied by a feeling of incomplete emptying").
-
Frequency & Urgency Detail: Instead of general terms, quantify frequency ("urinating every 30 minutes," "urinating more than 10 times a day") and urgency ("intense urge to urinate, difficult to delay").
-
Past UTI History: Provide more detail on past UTIs, including the causative organism (if known), treatment received, and the duration of symptoms. This information aids in treatment decisions and risk assessment.
-
Sexual History: While the initial note is sufficient, you could expand on this to include frequency of intercourse, use of barrier methods (condoms), and any recent changes in sexual partners. These aspects are crucial in understanding the potential source of the infection.
-
Hydration Habits: Elaborate on fluid intake; specify the types of fluids consumed and the approximate daily volume.
Objective: Enhancing the Physical Examination
The objective section can be further improved by adding details that rule out other potential causes:
-
Detailed Abdominal Exam: Include specific notes on palpation of the kidneys (to assess for any tenderness, suggesting pyelonephritis, a kidney infection) and a deeper abdominal assessment for other possible sources of symptoms.
-
Pelvic Exam Details: If a pelvic exam is performed, describe findings in more detail. Mention the presence or absence of any vaginal discharge, lesions, or tenderness.
-
Specific Urinalysis Findings: Include detailed urinalysis results, such as pH, specific gravity, presence of blood (hematuria) or crystals. The quantification of white blood cells and bacteria ("many," "few," "moderate") adds significant clinical information.
Assessment: Differentiating UTI Types and Complication Assessment
The assessment section can be enriched by differentiating various types of UTIs:
-
Complicated vs. Uncomplicated UTI: Clearly define why the UTI is classified as uncomplicated. The absence of risk factors (such as pregnancy, diabetes, indwelling catheters, or structural abnormalities) is essential to justify the uncomplicated designation.
-
Possible Causative Organisms: While E. coli is the most common, broaden the discussion to include other potential causative agents like Staphylococcus saprophyticus, Klebsiella pneumoniae, or Proteus mirabilis, especially if the patient has risk factors.
-
Differential Diagnoses: Briefly mention alternative diagnoses considered and why they were ruled out. For instance, interstitial cystitis, vulvovaginitis, or sexually transmitted infections could mimic UTI symptoms.
Plan: Detailed Treatment Strategy and Patient Education
The plan section can be strengthened by adding details about patient education:
-
Medication Details: Include the medication's mechanism of action, potential side effects (nausea, rash, diarrhea), and what to do if side effects occur.
-
Specific Fluid Recommendations: Instead of just "increase fluid intake," specify the recommended daily amount of fluid intake (e.g., "8-10 glasses of water").
-
Hygiene Practices: Detail recommended hygiene practices: wiping from front to back, avoiding harsh soaps, and maintaining cleanliness around the urethra.
-
Cranberry Juice: While the efficacy is debated, you could mention the possible role of cranberry juice in preventing recurrent UTIs (but emphasize that it is not a substitute for antibiotics).
-
Follow-up Instructions: Specify what to do if symptoms worsen or fail to improve, including contact information for the healthcare provider.
By expanding upon these sections with detailed information, the SOAP note becomes more informative, comprehensive, and optimized for better search engine visibility. The use of specific keywords like "dysuria," "frequency," "urgency," "urinalysis," "UTI," "E.coli," "antibiotics," "trimethoprim-sulfamethoxazole," "nitrofurantoin" and other medical terminology naturally enhances the note's SEO value. Remember to always maintain patient privacy and adhere to HIPAA guidelines when documenting patient information.
Latest Posts
Latest Posts
-
Asa Is Buying A Gift For His Mother
Mar 26, 2025
-
Super Size Me Movie Worksheet Answers
Mar 26, 2025
-
Pre Lab Video Coaching Activity Stretch Reflexes
Mar 26, 2025
-
Intrinsic Motivation Reflects Desires That Others Have
Mar 26, 2025
-
Label The Organs Based On The Hints Provided
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Soap Note For Urinary Tract Infection . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
