The Nurse Recognizes Which As Being True Of Cardioversion
Onlines
Mar 13, 2025 · 8 min read
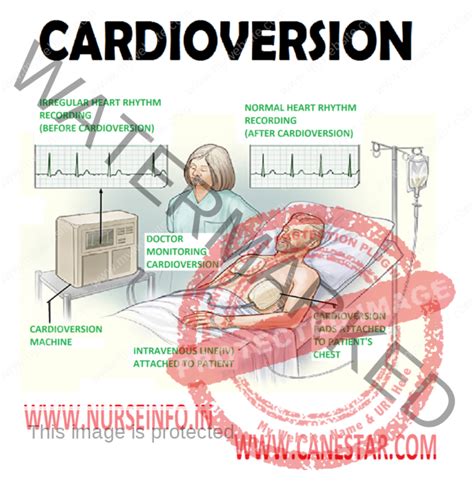
Table of Contents
The Nurse Recognizes Which as Being True of Cardioversion?
Cardioversion is a life-saving procedure used to restore a normal heart rhythm. It's a crucial intervention in various cardiac emergencies, but understanding its nuances is critical for nurses. This article will delve deep into the facts surrounding cardioversion, exploring what nurses need to know about its application, procedure, and potential complications. We will examine the key aspects nurses must recognize as true regarding cardioversion, focusing on patient assessment, preparation, and post-procedure care.
Understanding the Basics of Cardioversion
Cardioversion is a therapeutic procedure that uses synchronized electrical shocks to restore a normal heart rhythm. Unlike defibrillation, which is used in life-threatening situations like ventricular fibrillation or pulseless ventricular tachycardia, cardioversion is employed for organized but abnormal rhythms such as atrial fibrillation, atrial flutter, or supraventricular tachycardia (SVT). These rhythms, while not immediately life-threatening, can cause significant symptoms like palpitations, shortness of breath, dizziness, and chest pain, and can potentially lead to serious complications if left untreated.
Key Differences Between Cardioversion and Defibrillation
It's essential to distinguish between cardioversion and defibrillation. While both use electrical shocks, the crucial difference lies in synchronization:
-
Cardioversion: The electrical shock is delivered in synchrony with the patient's QRS complex (the ventricular depolarization wave on the ECG). This ensures that the shock is delivered during the ventricular contraction phase, minimizing the risk of inducing ventricular fibrillation.
-
Defibrillation: The electrical shock is delivered asynchronously, regardless of the QRS complex. This is necessary in situations where the heart's rhythm is chaotic and unsynchronized.
This synchronization aspect is a critical point nurses must recognize as true about cardioversion. The use of a synchronized mode is paramount to the safety and effectiveness of the procedure.
Patient Assessment Before Cardioversion
A thorough assessment is paramount before initiating cardioversion. The nurse plays a vital role in this process, gathering crucial information that will influence the procedure's success and the patient's safety.
1. ECG Interpretation: The Foundation of Cardioversion
Accurate ECG interpretation is the cornerstone of cardioversion. The nurse must confirm the presence of a rapid, organized rhythm that warrants cardioversion. This includes identifying the specific rhythm (e.g., atrial fibrillation, atrial flutter) and assessing its stability. Understanding the underlying rhythm dictates the approach to cardioversion and subsequent management.
2. Vital Signs Monitoring: A Continuous Assessment
Continuous monitoring of vital signs, including heart rate, blood pressure, respiratory rate, and oxygen saturation, is essential. These parameters provide baseline data and allow for early detection of any adverse reactions or complications during and after the procedure. Changes in these vital signs can indicate the effectiveness of cardioversion or potential issues requiring immediate intervention.
3. Medication History and Allergies: Preventing Adverse Reactions
A comprehensive medication history, including any anticoagulants (e.g., warfarin, apixaban, dabigatran), antiarrhythmics, or other medications that might interact with cardioversion or increase the risk of bleeding, is crucial. Identifying allergies, particularly to medications used for sedation or any potential reaction to the procedure itself, is equally vital.
4. Patient Education and Consent: Informed Decision-Making
Before cardioversion, the nurse should ensure the patient understands the procedure, its potential benefits and risks, and alternative treatment options. Obtaining informed consent is a crucial step, verifying the patient’s comprehension and voluntary agreement to undergo the procedure. Addressing patient anxiety and concerns is crucial for a successful outcome.
Preparing the Patient for Cardioversion
Careful preparation is key to a smooth and safe cardioversion procedure. The nurse plays a vital role in ensuring the patient is adequately prepared both physically and emotionally.
1. Skin Preparation: Ensuring Optimal Contact
The skin at the electrode placement sites (typically the anterior and posterior chest) needs to be cleaned thoroughly with an antiseptic solution. This ensures optimal electrical conductivity and minimizes the risk of burns or infection. Hair removal might be necessary at the electrode sites to facilitate proper contact and reduce impedance.
2. Electrode Placement: Precise Positioning for Effective Shock Delivery
Correct electrode placement is critical for effective cardioversion. The nurse should ensure that the pads are securely placed according to the cardioversion machine's instructions and the patient's body habitus. The specific placement depends on the machine used, but adhering to the manufacturer's guidelines is paramount.
3. Sedation and Analgesia: Managing Patient Discomfort
Cardioversion can be uncomfortable, so sedation and analgesia are often administered to minimize the patient’s discomfort and anxiety. The nurse's role involves assisting with administering these medications, monitoring their effects, and observing for any adverse reactions. The choice of sedatives depends on the patient's condition and other medical factors.
4. Monitoring Equipment: Continuous Observation and Response
Continuous monitoring of the ECG, vital signs, and oxygen saturation is maintained throughout the procedure. This enables immediate detection of any changes in the patient's condition and allows for prompt intervention if needed. The nurse remains vigilant during this stage, ready to respond to any complications.
The Cardioversion Procedure: A Step-by-Step Overview
The cardioversion procedure itself is relatively brief, but the nurse's role remains crucial in ensuring its safe and efficient execution.
1. Energy Level Selection: A Crucial Decision
The energy level used for cardioversion is determined by the type of rhythm and the patient's overall condition. Typically, synchronized cardioversion starts with lower energy levels (e.g., 50-100 joules), increasing the energy if necessary. This decision is usually made by the physician based on the ECG findings and patient response.
2. Shock Delivery: A Synchronized Intervention
The synchronized shock is delivered by the cardioversion machine. The nurse ensures that all personnel are clear of the patient and the equipment to prevent accidental injury from the electrical shock. Post-shock rhythm assessment is immediately performed.
3. Post-Shock Assessment: Immediate Evaluation and Response
Following the shock, immediate assessment of the patient’s rhythm, vital signs, and level of consciousness is crucial. If the cardioversion is successful, the normal heart rhythm should be restored. However, if the abnormal rhythm persists, the physician may decide to repeat the procedure with a higher energy level or consider alternative interventions.
4. Documentation: A Complete Record of the Procedure
Meticulous documentation of the entire process is essential. This includes the pre-cardioversion assessment, the energy levels used, the patient’s response to the shock, any medications administered, and the post-cardioversion assessment. This detailed documentation is vital for future medical care and legal purposes.
Post-Cardioversion Care: Monitoring and Recovery
Post-cardioversion care is crucial for monitoring the patient's recovery and preventing potential complications. The nurse's role in this phase involves close observation and timely intervention.
1. Continuous Monitoring: Detecting Potential Complications
Continuous ECG monitoring and vital signs monitoring are crucial in the immediate post-cardioversion period to detect any potential complications like recurrence of the abnormal rhythm, bradycardia, hypotension, or bleeding.
2. Assessing Neurological Status: Monitoring for Adverse Effects
Assessing the patient’s neurological status, including level of consciousness, orientation, and any signs of neurological deficits, is important. Sedatives used during the procedure might cause temporary neurological effects, which the nurse must monitor closely.
3. Managing Pain and Discomfort: Providing Relief
The patient might experience pain or discomfort at the electrode sites or generally. The nurse should administer analgesics as prescribed to manage this pain effectively.
4. Medication Management: Addressing Underlying Conditions
The nurse plays a crucial role in managing the patient’s medications, ensuring that all prescribed medications are administered correctly and on time. This includes anticoagulants or antiarrhythmics that might be necessary to maintain the normal rhythm or prevent recurrence.
5. Patient Education: Promoting Understanding and Compliance
Before discharge, the nurse should educate the patient about their condition, the importance of medication adherence, potential complications, and signs and symptoms to watch for. Encouraging lifestyle modifications, such as diet and exercise, is crucial to promote long-term health.
Potential Complications of Cardioversion: Recognizing and Managing Risks
While generally safe, cardioversion carries potential risks that nurses must be aware of.
1. Recurrence of Arrhythmia: A Possible Outcome
The abnormal heart rhythm might recur despite successful cardioversion. This underscores the importance of ongoing monitoring and appropriate medication management.
2. Bleeding: A Risk Associated with Anticoagulation
Patients on anticoagulants are at higher risk of bleeding, especially at the electrode sites. Close monitoring for bleeding and appropriate management are essential.
3. Burns: A Potential Side Effect of Electrode Placement
Burns can occur at the electrode placement sites due to poor skin preparation or improper electrode placement. Careful skin preparation and electrode placement technique are crucial in minimizing this risk.
4. Stroke: A Rare but Serious Complication
In patients with atrial fibrillation, cardioversion carries a small risk of dislodging blood clots, potentially leading to a stroke. Pre-cardioversion anticoagulation is often necessary to mitigate this risk.
5. Myocardial Damage: A Rare but Serious Possibility
In rare instances, cardioversion might cause myocardial damage. This risk is minimized by careful patient selection and appropriate energy levels.
Conclusion: The Nurse's Vital Role in Cardioversion
Cardioversion is a vital intervention in managing various cardiac arrhythmias. The nurse plays a crucial role throughout the entire process, from pre-procedure assessment and preparation to post-procedure monitoring and patient education. A deep understanding of the procedure's intricacies, potential complications, and effective management strategies is essential for ensuring patient safety and optimal outcomes. The nurse's vigilance and expertise are indispensable in delivering safe and effective cardioversion, improving patient outcomes, and contributing to the overall success of this life-saving procedure. By recognizing the truths outlined in this article, nurses can effectively contribute to the safe and efficient delivery of cardioversion, ultimately ensuring optimal patient care.
Latest Posts
Latest Posts
-
How To Find Dod Id Number In Outlook
Mar 13, 2025
-
Which Of The Following Statements Regarding Anaphylaxis Is Correct
Mar 13, 2025
-
Water Water Everywhere But Please Dont Give Iv Answer Key
Mar 13, 2025
-
Functions And Slope Quick Check Answer Key
Mar 13, 2025
-
What Process Occurs In Structure H
Mar 13, 2025
Related Post
Thank you for visiting our website which covers about The Nurse Recognizes Which As Being True Of Cardioversion . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
