Tina Jones Comprehensive Assessment Shadow Health Documentation
Onlines
Mar 04, 2025 · 6 min read
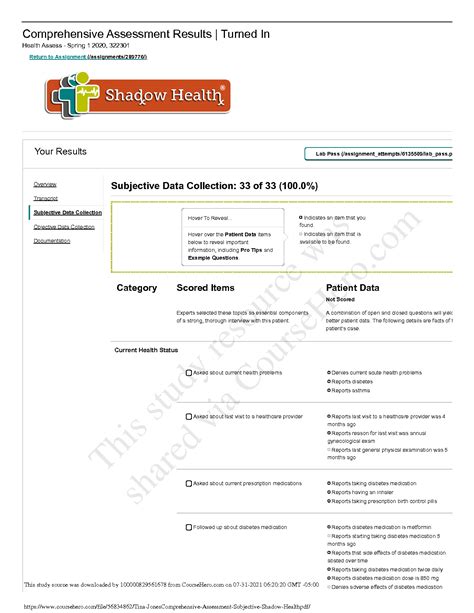
Table of Contents
Tina Jones Comprehensive Assessment: A Deep Dive into Shadow Health Documentation
Shadow Health's Tina Jones comprehensive assessment offers a robust platform for nursing students to practice their assessment skills in a risk-free environment. This detailed simulation allows students to hone their abilities in patient history taking, physical examination techniques, and diagnostic reasoning. This comprehensive guide delves into the various aspects of documenting a Tina Jones assessment, offering insights and tips for maximizing learning and achieving accurate, thorough documentation.
Understanding the Shadow Health Tina Jones Simulation
The Tina Jones simulation isn't just about memorizing facts; it's about developing critical thinking and clinical judgment. It presents a virtual patient with a complex medical history, allowing students to practice a holistic approach to patient care. Successfully navigating the simulation necessitates a deep understanding of:
1. Patient History: The Foundation of Assessment
The patient history forms the cornerstone of any successful assessment. With Tina Jones, you’ll gather information through:
-
Subjective Data: This encompasses the patient's own account of their symptoms, medical history, family history, social history, and lifestyle factors. Thorough questioning is paramount. Don't be afraid to ask follow-up questions to clarify vague answers or explore potential connections between seemingly unrelated symptoms. Pay close attention to the patient's chief complaint and ensure you document it accurately.
-
Objective Data: This refers to the observable and measurable findings from the physical examination. Accurate documentation of objective data is crucial. Remember to record vital signs, auscultation findings (heart and lung sounds), palpation findings (e.g., tenderness, masses), and any other relevant physical examination findings. Be precise and detailed in your descriptions. Instead of writing "abnormal lung sounds," specify "crackles heard in the right lower lobe."
Pro-Tip: Practice using the SOAP (Subjective, Objective, Assessment, Plan) note format. This widely used structure ensures organized and comprehensive documentation. This helps you maintain a clear and logical flow of information, facilitating easier comprehension and reducing the risk of overlooking vital details.
2. Physical Examination: A Hands-On Approach (Virtually)
The physical exam section of the Tina Jones assessment requires meticulous attention to detail. You'll need to demonstrate proficiency in:
-
General Appearance: Note the patient's overall appearance, including their level of consciousness, comfort level, and any obvious signs of distress.
-
Vital Signs: Accurately record and interpret vital signs like temperature, pulse, blood pressure, respiratory rate, and oxygen saturation. Understanding the implications of abnormal vital signs is crucial for formulating a diagnosis.
-
Head-to-Toe Assessment: Systematically examine each body system, documenting your findings precisely. For instance, when assessing the cardiovascular system, carefully listen to heart sounds, noting any murmurs, gallops, or irregularities. Similarly, during respiratory assessment, listen for wheezes, crackles, or rhonchi. Document the location and characteristics of any abnormal sounds.
-
Neurological Assessment: Assess the patient's mental status, cranial nerves, motor strength, sensory function, and reflexes. Be sure to use standardized scales, like the Glasgow Coma Scale (GCS) when appropriate.
Pro-Tip: Review anatomical diagrams and practice your physical exam techniques before attempting the simulation. Familiarity with the proper procedures will significantly improve your performance and the accuracy of your documentation. Consider using practice models or reviewing videos to refine your skills.
3. Diagnostic Reasoning: Connecting the Dots
This is where the true challenge lies. Based on the subjective and objective data collected, you must formulate a differential diagnosis – a list of possible diagnoses ranked in order of likelihood. To excel in this aspect:
-
Analyze the Data: Carefully review all collected data, looking for patterns and correlations. For example, a patient complaining of chest pain coupled with shortness of breath and abnormal lung sounds might suggest a respiratory or cardiovascular issue.
-
Prioritize Diagnoses: Based on the prevalence, severity, and probability of each condition, prioritize your differential diagnosis. This shows clinical reasoning and decision-making skills.
-
Consider Risk Factors: Take the patient's age, medical history, lifestyle factors, and social history into account when prioritizing diagnoses.
Pro-Tip: Utilize resources like diagnostic decision trees and clinical practice guidelines to refine your diagnostic reasoning skills. Strengthening your knowledge base through continuous learning is essential for accurate diagnosis.
4. Developing a Treatment Plan: The Plan of Care
Once you've formulated a diagnosis (or a prioritized list of differential diagnoses), you must develop a comprehensive treatment plan. This plan should include:
-
Pharmacological Interventions: If medication is indicated, specify the medication, dosage, route of administration, and frequency. Justify your medication choices based on the patient's condition and potential side effects.
-
Non-Pharmacological Interventions: Include non-pharmacological interventions such as patient education, lifestyle modifications, and referrals to other healthcare professionals. Consider the patient's preferences and cultural background when planning interventions.
-
Follow-up Care: Outline a plan for follow-up care, including the need for further investigations, referrals, or monitoring.
Pro-Tip: Consult reliable sources like medical textbooks and clinical guidelines to ensure the accuracy and appropriateness of your treatment plan. Always prioritize patient safety and well-being.
Mastering Tina Jones Documentation: Tips and Strategies
Accurate and comprehensive documentation is crucial. Here are some key strategies for success:
1. Use Clear and Concise Language:
Avoid medical jargon and ensure your documentation is understandable to other healthcare professionals. Use precise language and avoid ambiguity.
2. Maintain Objective and Subjective Clarity:
Clearly distinguish between subjective and objective findings. Label them appropriately to maintain clear separation within your documentation.
3. Utilize Standard Abbreviations and Terminology:
Employ standardized abbreviations and terminology to ensure consistency and clarity in your documentation. However, only use widely accepted and understood abbreviations to avoid confusion.
4. Follow a Consistent Format:
Adhere to a consistent format for your documentation. The SOAP note format is widely recommended for its organization and clarity. Maintaining this consistency will greatly aid the review process, aiding comprehension.
5. Double-Check for Accuracy:
Before submitting your documentation, meticulously review it for accuracy and completeness. Ensure that all relevant data has been included and that there are no inconsistencies or errors.
6. Practice Regularly:
Consistent practice is key to mastering the Tina Jones comprehensive assessment. Regularly engaging with the simulation will solidify your understanding and build confidence in your clinical skills.
Beyond the Simulation: Applying Your Knowledge
The Tina Jones simulation is a valuable tool, but its true worth lies in its ability to prepare you for real-world clinical practice. The skills and knowledge gained from this simulation should be applied to every patient interaction.
Remember to:
- Continuously learn and update your knowledge: The medical field is constantly evolving. Stay abreast of the latest advances and best practices.
- Develop critical thinking and clinical judgment: The ability to analyze data, formulate diagnoses, and develop treatment plans is essential for successful patient care.
- Practice effective communication: Clear and empathetic communication with patients is crucial for building trust and rapport, ensuring effective care.
The Tina Jones comprehensive assessment within Shadow Health is not just a simulation; it’s a powerful learning tool that fosters critical thinking, diagnostic reasoning, and documentation skills—essential competencies for aspiring healthcare professionals. By mastering this simulation and applying its lessons to real-world scenarios, you'll be well-equipped to provide compassionate and effective patient care.
Latest Posts
Latest Posts
-
Pn Pediatric Nursing Online Practice 2023 A
Mar 04, 2025
-
Quiz 6 2 Proving Triangles Are Similar
Mar 04, 2025
-
Worksheet 10 5 Chapter 10 Crossword Puzzzle
Mar 04, 2025
-
Write The Formula Formula Unit For The Following Compounds
Mar 04, 2025
-
Case Study Celiac Disease Answer Key
Mar 04, 2025
Related Post
Thank you for visiting our website which covers about Tina Jones Comprehensive Assessment Shadow Health Documentation . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
