Tina Jones Respiratory Shadow Health Transcript
Onlines
Mar 24, 2025 · 7 min read
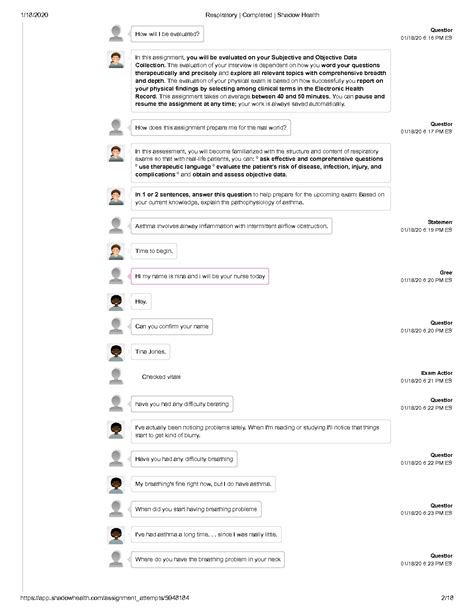
Table of Contents
Tina Jones Respiratory Shadow Health Transcript: A Comprehensive Guide for Students
The Tina Jones Respiratory Shadow Health simulation is a valuable tool for nursing students to practice their assessment and treatment skills in a safe, virtual environment. This comprehensive guide delves deep into a possible transcript from the simulation, analyzing key aspects of the assessment, diagnosis, and management of Tina Jones' respiratory condition. We'll explore the crucial elements of the patient interview, physical examination findings, and the rationale behind the chosen interventions. Remember, this is a sample transcript; your actual experience may vary.
The Patient Interview: Uncovering Tina's Story
The initial interaction with Tina Jones is critical. A thorough patient history provides valuable clues about the underlying cause of her respiratory distress. Key areas to explore include:
Chief Complaint:
Tina's chief complaint might be shortness of breath (dyspnea), cough, chest pain, or a combination of these. The severity and duration of these symptoms are crucial pieces of information. For example, she might describe her shortness of breath as being worse with exertion or at rest. A persistent cough could indicate a chronic condition, while a sudden onset could suggest an acute infection.
History of Present Illness (HPI):
This section focuses on a detailed timeline of her symptoms. Consider the following prompts and possible responses:
- Onset: When did the symptoms begin? Was it sudden or gradual?
- Location: Where is the discomfort or shortness of breath felt? Is it localized to the chest or more generalized?
- Character: Describe the cough (productive or non-productive, dry or wet, and the character of the sputum). Describe the chest pain (sharp, dull, aching, stabbing). How would Tina describe her shortness of breath?
- Aggravating/Alleviating Factors: What makes the symptoms worse or better? Does lying down worsen the dyspnea (orthopnea)? Does sitting upright or using pillows help (orthopnea)? Does activity exacerbate the symptoms? Does any medication provide relief?
- Timing: How frequently do the symptoms occur? Are they continuous or intermittent?
- Severity: How severe are the symptoms on a scale of 1-10?
- Associated Symptoms: Are there any other symptoms, such as fever, chills, fatigue, muscle aches, nausea, vomiting, or changes in bowel or bladder habits? These can provide vital clues about the underlying condition.
Past Medical History (PMH):
Tina's PMH is essential for context. Pre-existing conditions, such as asthma, COPD, heart failure, or previous respiratory infections, can significantly influence her current condition. Past surgeries, hospitalizations, and allergies should also be documented.
Family History (FH):
A family history of respiratory illnesses, such as asthma, lung cancer, or cystic fibrosis, could increase the risk of similar conditions in Tina.
Social History (SH):
Lifestyle factors play a vital role. Smoking history (pack-years), exposure to environmental pollutants (dust, fumes, asbestos), occupation, and alcohol and drug use are all important considerations. This information can shed light on potential causes of her respiratory problems.
Medication History:
A thorough review of current medications, including over-the-counter (OTC) drugs and herbal supplements, is crucial. Some medications can interact with or worsen respiratory conditions.
Allergies:
Document any allergies to medications, food, or environmental substances. This is vital to prevent adverse reactions during treatment.
The Physical Examination: Observing and Assessing Tina
The physical examination is where you put your clinical skills to the test. Key elements of a respiratory assessment include:
General Appearance:
Observe Tina's overall appearance. Note her level of distress, respiratory rate, and use of accessory muscles (e.g., neck muscles, intercostal muscles) for breathing. Cyanosis (bluish discoloration of the skin and mucous membranes) indicates poor oxygenation.
Vital Signs:
Accurate vital signs are fundamental. Pay close attention to:
- Heart Rate (HR): Tachycardia (increased HR) might indicate hypoxia or respiratory distress.
- Respiratory Rate (RR): Tachypnea (increased RR) suggests respiratory compromise. Observe the rhythm and depth of breathing.
- Blood Pressure (BP): Hypotension (low BP) can be a consequence of severe respiratory distress.
- Temperature: Fever might suggest an infection.
- Oxygen Saturation (SpO2): Low SpO2 (hypoxemia) indicates insufficient oxygen levels in the blood.
Auscultation:
Using a stethoscope, listen to Tina's lungs. Listen for abnormal breath sounds such as:
- Wheezes: High-pitched whistling sounds, often indicating bronchospasm or airway narrowing.
- Rales (Crackles): Crackling or bubbling sounds, often indicating fluid in the alveoli (air sacs).
- Rhonchi: Low-pitched rumbling sounds, usually associated with mucus in the larger airways.
- Absent Breath Sounds: Absence of breath sounds in certain areas could suggest atelectasis (collapsed lung) or pleural effusion (fluid buildup around the lungs).
Palpation:
Palpate Tina's chest wall for tenderness, crepitus (a crackling sensation), and tactile fremitus (vibrations felt when the patient speaks).
Percussion:
Percuss Tina's chest to assess lung resonance. Dullness can indicate fluid or consolidation (areas of lung tissue filled with fluid or inflammatory cells).
Diagnosis and Management: Putting It All Together
Based on the history and physical examination, you'll formulate a differential diagnosis. Possible diagnoses for Tina Jones’ respiratory symptoms could include:
- Pneumonia: Infection of the lungs.
- Asthma: Airway inflammation and bronchospasm.
- Chronic Obstructive Pulmonary Disease (COPD): Progressive lung disease characterized by airflow limitation.
- Acute Bronchitis: Inflammation of the bronchi.
- Pleurisy: Inflammation of the pleura (lining of the lungs).
- Pulmonary Embolism: Blood clot in the lungs.
- Heart Failure: Inability of the heart to pump enough blood to meet the body's needs.
The chosen management strategy depends heavily on the suspected diagnosis. This might involve:
- Oxygen Therapy: Supplemental oxygen to improve oxygen saturation.
- Bronchodilators: Medications to relax the airways and improve breathing (e.g., albuterol).
- Corticosteroids: Anti-inflammatory medications to reduce airway inflammation (e.g., prednisone).
- Antibiotics: If an infection is suspected (e.g., pneumonia).
- Fluid Management: In cases of heart failure or pulmonary edema.
- Further Investigations: Chest X-ray, arterial blood gas (ABG) analysis, sputum culture, electrocardiogram (ECG).
Interpreting the Results: Putting the Pieces Together
The results of any diagnostic tests, such as a chest X-ray, should be carefully analyzed in conjunction with the clinical findings. For example:
- Chest X-ray: Could reveal pneumonia (consolidation), COPD (hyperinflation), or pleural effusion (fluid in the pleural space).
- ABG analysis: Provides objective data on blood oxygen levels, carbon dioxide levels, and pH, which are essential for assessing respiratory function.
- Sputum Culture: Identifies the specific bacteria or virus causing an infection (if any).
The Importance of Patient Education: Empowering Tina
Patient education is a vital part of Tina's care. Teach her about her condition, the importance of medication adherence, and lifestyle modifications that might improve her respiratory health. This could involve:
- Medication instructions: Clearly explain how to take her medications, possible side effects, and when to contact her healthcare provider.
- Breathing techniques: Teach her techniques such as pursed-lip breathing to improve oxygenation and reduce dyspnea.
- Activity modification: Advise her to pace her activities to avoid exacerbating her symptoms.
- Smoking cessation: If applicable, provide resources and support to help her quit smoking.
- Follow-up care: Schedule a follow-up appointment to monitor her progress and address any concerns.
Reflecting on the Simulation: Learning and Growth
After completing the simulation, take time to reflect on your performance. Consider the following questions:
- Did you gather a complete and accurate patient history?
- Were your physical examination findings thorough and accurate?
- Did you formulate a reasonable differential diagnosis?
- Did you choose appropriate interventions?
- Did you effectively communicate with the patient and educate her about her condition?
Using the Shadow Health platform to simulate patient interactions can greatly improve your critical thinking skills, patient assessment techniques, and overall clinical judgment. Regular practice and reflection are crucial for mastering the art of nursing.
This extensive guide provides a framework for understanding a possible Tina Jones Respiratory Shadow Health transcript. Remember that each simulation will be unique and will require careful observation, critical thinking, and a thorough understanding of respiratory physiology and pathology. This in-depth exploration of the possible scenario aims to equip nursing students with the knowledge and confidence to approach similar cases in real-world clinical settings. The key is to combine theoretical knowledge with practical application – a skill honed through the repetition and reflection provided by virtual simulations like Shadow Health.
Latest Posts
Latest Posts
-
Summary Of Chapter 21 Of The Giver
Mar 26, 2025
-
When The Emperor Was Divine Quotes
Mar 26, 2025
-
Dell Roadmap Of A Digital Supply Chain Transformation
Mar 26, 2025
-
Catcher In The Rye Chapter 15 Summary
Mar 26, 2025
-
Factors That Lead To Personal Offenses Include
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Tina Jones Respiratory Shadow Health Transcript . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
