To Which Patient Might The Nurse Apply A Physical Restraint
Onlines
Apr 01, 2025 · 6 min read
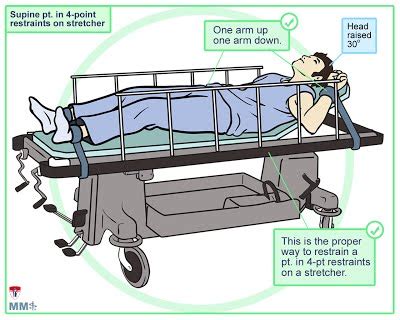
Table of Contents
To Which Patient Might the Nurse Apply a Physical Restraint?
The use of physical restraints in healthcare settings is a complex and sensitive issue. While they can be necessary to ensure patient safety and the safety of others, their application should always be a last resort, preceded by thorough assessment and exploration of less restrictive alternatives. This article delves into the circumstances under which a nurse might consider applying a physical restraint, emphasizing the ethical and legal considerations surrounding this practice.
Understanding Physical Restraints
Before examining specific patient scenarios, it's crucial to define what constitutes a physical restraint. Physical restraints are any device, material, or equipment that restricts a patient's freedom of movement. This includes, but isn't limited to:
- Wrist restraints: Straps or cuffs that restrict movement of the wrists.
- Ankle restraints: Similar to wrist restraints, but for the ankles.
- Vest restraints: A jacket-like restraint that restricts torso movement.
- Belt restraints: A strap that secures the patient to a bed or chair.
- Mitts: Devices that cover the hands, preventing scratching or pulling at medical equipment. These are considered less restrictive than wrist restraints.
It's important to differentiate between physical restraints and other interventions that might limit movement but aren't considered restraints. These include:
- Side rails: While side rails can help prevent falls, they aren't generally considered restraints unless they are used to actively restrict a patient's movement.
- Adaptive equipment: Devices like walkers and wheelchairs assist with mobility, and are not considered restraints.
- Protective clothing: Clothing used to prevent skin breakdown or self-harm, such as elbow and knee pads, are usually not considered restraints.
Legal and Ethical Considerations
The application of physical restraints is governed by strict legal and ethical guidelines. Consent is paramount. While in some emergency situations, immediate restraint might be necessary before obtaining consent, this must be justified and documented thoroughly. The use of restraints without proper consent can lead to legal repercussions.
Least restrictive means: Healthcare professionals are obligated to use the least restrictive means necessary to ensure patient safety. This means exploring all alternatives to restraints before resorting to them. These alternatives could include:
- Increased observation: More frequent checks on the patient.
- Environmental modifications: Removing tripping hazards, providing adequate lighting, and ensuring easy access to assistive devices.
- Behavioral interventions: Techniques like redirection, distraction, and calming communication.
- Medication: In some cases, medication can help manage disruptive behaviors.
- Sensory interventions: Using calming music, aromatherapy, or other sensory inputs.
Documentation: Meticulous documentation is vital. The nurse must document the rationale for using restraints, the type of restraint used, the frequency of monitoring, any adverse effects, and the patient's response. This documentation serves as a legal and ethical record of the intervention.
Patient Scenarios Where Restraints Might Be Considered
The decision to apply physical restraints should never be taken lightly. It requires a thorough assessment of the patient's condition and the potential risks. Here are some scenarios where restraints might be considered, but always with a strong emphasis on exploring alternatives first:
1. Risk of Falls
Patients at high risk of falls, particularly those with cognitive impairment, dementia, or impaired mobility, may require restraints to prevent injuries. However, before resorting to restraints, the nurse should implement fall prevention strategies like bed alarms, floor mats, and regular monitoring. Restraints should only be used as a last resort if fall prevention measures fail to mitigate the risk.
2. Self-Harm or Harm to Others
Patients exhibiting self-harm behaviors, such as pulling out intravenous lines or injuring themselves, might require restraints to protect them from harm. Similarly, patients who pose a risk of harm to others, either through aggressive behavior or disorientation, might require restraints to ensure the safety of staff and other patients. It's crucial to assess the root cause of the behavior and explore less restrictive options, like de-escalation techniques and one-on-one supervision.
3. During Medical Procedures
In certain medical procedures, temporary restraints might be necessary to ensure the patient's safety and the success of the procedure. For instance, restraints might be used during an MRI scan to prevent movement that could blur the images. However, the use of restraints should be minimal, and the patient should be informed and consent obtained (where possible) before the procedure.
4. Post-Operative Patients
Some post-operative patients may require temporary restraints to prevent dislodging of tubes, drains, or dressings. Again, less restrictive methods should be considered first, such as protective clothing or increased monitoring. Restraints should only be applied if these methods are insufficient.
5. Patients with Delirium or Agitation
Patients experiencing delirium or severe agitation, often associated with illness or medication side effects, might require temporary restraints to prevent self-harm or injury to others. However, managing underlying causes, such as pain, infection, or medication side effects, is crucial. Non-pharmacological interventions, like calming music or reorientation, should be attempted before resorting to restraints.
6. Patients with Dementia
Patients with dementia can exhibit unpredictable behaviors that may put themselves or others at risk. Restraints should be considered a last resort, after thorough evaluation and exploration of other strategies, such as:
- Environmental adjustments: Creating a safe and predictable environment.
- Cognitive stimulation: Engaging in activities that stimulate the patient's mind.
- Behavioral management techniques: Using techniques to redirect or calm the patient.
- Medication (under physician's orders): To manage agitation or aggression.
Monitoring and Documentation
Once a physical restraint is applied, the nurse must carefully monitor the patient's condition. This includes:
- Regularly checking for skin breakdown: Restraints can restrict blood flow and cause pressure sores.
- Assessing for discomfort or pain: The patient should be assessed regularly for any signs of discomfort.
- Monitoring vital signs: Changes in vital signs could indicate complications.
- Observing for signs of agitation or distress: The nurse should look for signs that the restraint is causing the patient undue stress.
- Documenting all observations: Any changes in the patient's condition should be thoroughly documented.
The frequency of monitoring depends on the type of restraint and the patient's condition but should be at least every 15-30 minutes. The nurse must also document the rationale for using restraints, the type of restraint used, the duration, the patient's response, and any adverse effects.
Alternatives to Physical Restraints
As emphasized throughout this article, using physical restraints should be considered only as a last resort. Numerous alternatives can often effectively manage patient safety without resorting to physical restraints. These alternatives must always be thoroughly explored and documented. They include, but are not limited to:
- Increased supervision: One-on-one monitoring by trained staff.
- Environmental modifications: Removing hazards, ensuring adequate lighting, and providing assistive devices.
- Behavioral interventions: Calm communication, redirection, distraction, and de-escalation techniques.
- Therapeutic activities: Engaging the patient in activities tailored to their interests and abilities.
- Sensory strategies: Using calming music, aromatherapy, or other sensory inputs to reduce anxiety.
- Family involvement: Involving family members in the care of the patient, as their presence can be calming and reassuring.
- Medication (as ordered by a physician): Medication may be necessary in some cases to manage agitation or disruptive behaviors.
In conclusion, the use of physical restraints in healthcare is a critical issue requiring careful consideration and adherence to legal and ethical guidelines. The nurse's role is to prioritize patient safety while minimizing the use of restraints, employing alternative strategies wherever possible, and meticulously documenting all aspects of restraint use. Every situation should be approached with a patient-centered approach, striving to maintain the patient's dignity and autonomy while ensuring safety for both the patient and others. The decision to apply a restraint is not taken lightly and requires professional judgment, careful assessment, and a strong commitment to ethical practice.
Latest Posts
Latest Posts
-
For Each Scenario Calculate The Income Elasticity Of Demand
Apr 02, 2025
-
What Do Internship Programs Typically Accomplish
Apr 02, 2025
-
An Amusement Park Attraction Has A Sign That Indicates
Apr 02, 2025
-
What Characteristic Makes English A Deep Alphabetic Orthography
Apr 02, 2025
-
Brecht On Theatre The Development Of An Aesthetic
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about To Which Patient Might The Nurse Apply A Physical Restraint . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
