Which Intervention Does A Nurse Implement For Clients With Empyema
Onlines
Mar 19, 2025 · 7 min read
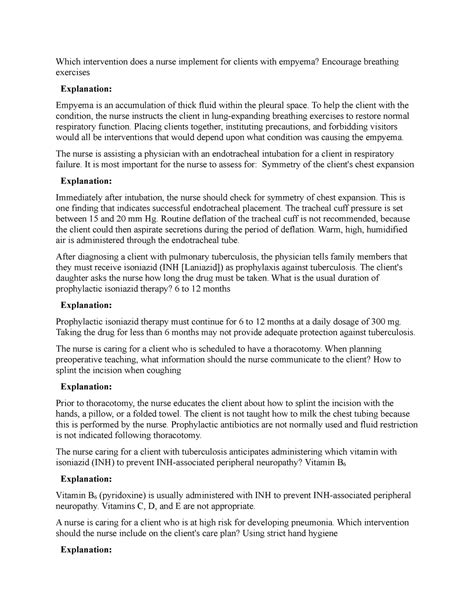
Table of Contents
Which Interventions Does a Nurse Implement for Clients with Empyema?
Empyema, a collection of pus in the pleural space, is a severe complication often arising from pneumonia, lung abscesses, or thoracic surgery. Its presence necessitates prompt and comprehensive nursing interventions to prevent life-threatening complications and improve patient outcomes. This article delves into the multifaceted nursing care required for clients with empyema, encompassing assessment, diagnostic testing, pharmacological management, procedural support, and crucial patient education.
Assessing the Client with Empyema: A Multifaceted Approach
Accurate and timely assessment is the cornerstone of effective empyema management. The nurse's role begins with a thorough evaluation of the patient's history and presenting symptoms. This includes:
1. History Taking:
- Recent Infections: Elicit a detailed history of recent respiratory infections, including pneumonia, bronchitis, or tuberculosis, as these are common precursors to empyema.
- Surgical History: Inquire about any recent thoracic surgeries, as they can increase the risk of empyema development.
- Immunocompromised Status: Determine if the patient has any underlying conditions that compromise their immune system, such as HIV/AIDS, diabetes, or cancer, as these significantly impact the body's ability to fight infection.
- Symptom Onset and Progression: Document the onset and progression of symptoms, including fever, chills, cough (productive or non-productive), dyspnea (shortness of breath), pleuritic chest pain, and fatigue. Note the severity and duration of each symptom.
2. Physical Examination:
A comprehensive physical examination is crucial for detecting the signs and symptoms of empyema. This involves:
- Vital Signs: Closely monitor vital signs, specifically paying attention to fever (often high-grade), tachycardia (rapid heart rate), tachypnea (rapid breathing rate), and decreased oxygen saturation. These indicate the severity of the infection and the body's response to it.
- Respiratory Assessment: Auscultate the lungs for decreased or absent breath sounds over the affected area, indicating pleural fluid accumulation. Note the presence of crackles, wheezes, or bronchial breath sounds, which can signify associated pneumonia or lung consolidation.
- Chest Examination: Inspect the chest for asymmetry, indicating possible pleural effusion or lung collapse. Palpate the chest for tenderness, decreased tactile fremitus (vibrations felt during speech), and chest wall expansion limitations.
- Cardiovascular Assessment: Assess for signs of cardiovascular compromise, such as tachycardia, hypotension, and peripheral edema, which can occur due to the impact of empyema on cardiac function.
- Neurological Assessment: Assess the patient's mental status, noting any signs of confusion or altered consciousness, particularly in cases of severe infection or septic shock.
3. Diagnostic Testing:
The nurse plays a pivotal role in preparing the patient for and assisting with various diagnostic tests to confirm the diagnosis and guide treatment. These include:
- Chest X-Ray: This is typically the first imaging test performed. It reveals the presence of pleural effusion and helps to assess its size and location. The nurse explains the procedure, positions the patient appropriately, and ensures proper image acquisition.
- Computed Tomography (CT) Scan: A CT scan provides more detailed images of the pleural space, allowing for better visualization of the empyema collection, its extent, and any associated lung pathology. The nurse prepares the patient for the scan, including instructions about any necessary contrast agents and potential side effects.
- Thoracentesis: This procedure involves inserting a needle into the pleural space to aspirate fluid for analysis. The nurse assists the physician during the procedure, monitoring the patient's vital signs, ensuring proper sterile technique, and providing emotional support. The collected fluid is sent to the laboratory for analysis, including Gram stain, culture, and sensitivity testing to identify the causative organism and guide antibiotic therapy.
- Pleural Fluid Analysis: The nurse ensures that the collected pleural fluid is appropriately labeled and transported to the laboratory for analysis, which includes identifying the type of fluid, determining the presence of pus, identifying the causative organism, and measuring the fluid's pH and lactate dehydrogenase (LDH) levels. These findings are crucial in determining the nature and severity of the empyema.
Nursing Interventions for Empyema Management
Nursing interventions for empyema are multifaceted and focus on addressing the underlying infection, supporting respiratory function, and managing patient comfort.
1. Pharmacological Interventions:
- Antibiotics: Broad-spectrum antibiotics are initially prescribed to cover a wide range of potential pathogens. Once the culture and sensitivity results are available, the antibiotics are tailored to target the specific causative organism. The nurse administers the antibiotics as prescribed, monitors for allergic reactions and adverse effects, and educates the patient about the importance of completing the entire course of treatment.
- Analgesics: Pain management is crucial due to the pleuritic chest pain often associated with empyema. The nurse assesses pain levels, administers analgesics as prescribed (e.g., opioids, NSAIDs), and monitors for pain relief and any side effects.
- Antipyretics: Fever is a common symptom of empyema. The nurse administers antipyretics (e.g., acetaminophen) to reduce fever and improve patient comfort. Close monitoring of temperature is essential.
2. Respiratory Support:
- Oxygen Therapy: Supportive oxygen therapy is frequently necessary to maintain adequate oxygen saturation levels. The nurse monitors oxygen saturation using pulse oximetry, adjusts oxygen flow rates as prescribed, and ensures that the patient tolerates oxygen therapy well.
- Chest Physiotherapy: Techniques such as deep breathing exercises, coughing, and incentive spirometry are encouraged to help expand the lungs and mobilize secretions. The nurse instructs the patient on proper techniques and monitors their effectiveness.
- Mechanical Ventilation: In severe cases, mechanical ventilation may be required to support respiratory function. The nurse monitors ventilator settings, assesses the patient's respiratory status, and provides meticulous respiratory care.
3. Procedural Interventions:
- Chest Tube Insertion: Chest tube insertion is a common procedure for draining the empyema fluid. The nurse assists the physician during the procedure, ensuring proper sterile technique and monitoring the patient's vital signs. Post-procedure, the nurse monitors chest tube drainage, assesses for air leaks, and provides meticulous wound care.
- Video-Assisted Thoracoscopic Surgery (VATS): VATS is a minimally invasive surgical procedure used to drain the empyema and debride the infected pleural space. The nurse prepares the patient pre-operatively, provides post-operative care, monitors for complications such as bleeding and infection, and supports the patient's recovery.
- Open Thoracotomy: Open thoracotomy, a more invasive procedure, may be necessary in cases where VATS is not effective. The nurse's role in the pre-operative, intra-operative, and post-operative phases is extensive, encompassing patient education, preparation, monitoring, and post-operative care, including pain management and respiratory support.
4. Nutritional Support:
Adequate nutrition is essential for healing and recovery. The nurse assesses the patient's nutritional status, encourages a high-protein, high-calorie diet, and assists with feeding if necessary. Nutritional support may include enteral or parenteral nutrition in cases of significant nutritional deficits.
5. Patient Education:
Patient education is crucial for successful management of empyema. The nurse educates the patient about:
- Disease Process: Clearly explaining empyema, its causes, and potential complications.
- Medication Regimen: Thoroughly explaining the purpose, dosage, and potential side effects of prescribed medications.
- Respiratory Therapy: Instructing the patient on proper deep breathing exercises, coughing techniques, and incentive spirometry.
- Wound Care: Providing instructions on proper wound care if a chest tube is in place or if surgery has been performed.
- Follow-up Care: Emphasizing the importance of attending follow-up appointments and reporting any changes in condition to their healthcare provider.
- Infection Prevention: Educating the patient on measures to prevent future infections, such as practicing good hand hygiene and receiving recommended vaccinations.
Monitoring for Complications
Close monitoring for potential complications is paramount. These include:
- Respiratory Failure: Monitor for signs of respiratory distress, such as increased work of breathing, hypoxemia, and hypercapnia.
- Septic Shock: Assess for signs of septic shock, including hypotension, tachycardia, tachypnea, and altered mental status.
- Pleural Space Fibrosis: Observe for persistent pleural thickening and restricted lung expansion.
- Lung Abscess: Monitor for signs of lung abscess, such as persistent fever, cough with purulent sputum, and chest pain.
- Empyema Recurrence: Emphasize the importance of follow-up care to detect and treat any recurrence.
Conclusion: A Holistic Approach to Empyema Care
Empyema management requires a multidisciplinary approach, with the nurse playing a crucial role in assessment, intervention, and patient education. By implementing comprehensive nursing interventions, including meticulous monitoring, effective medication administration, respiratory support, procedural assistance, and patient education, nurses contribute significantly to improving patient outcomes and preventing life-threatening complications associated with this severe condition. A holistic approach, emphasizing patient comfort, emotional support, and adherence to the treatment plan, ensures the best possible recovery. The nurse's dedication to individualized care is vital in navigating the complexities of empyema and guiding the patient toward a successful recovery.
Latest Posts
Latest Posts
-
Student Exploration Coral Reefs 2 Biotic Factors Answer Key
Mar 20, 2025
-
Assignment 5 2 Skeletal System Case Studies
Mar 20, 2025
-
Lord Of Flies Chapter 4 Summary
Mar 20, 2025
-
Which Of These Is Correct About Identity Theft
Mar 20, 2025
-
La Pelicula Mala La Historia Del Cine
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about Which Intervention Does A Nurse Implement For Clients With Empyema . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
