While Transferring A Patient To Als Staff Interference Should Be
Onlines
Mar 29, 2025 · 5 min read
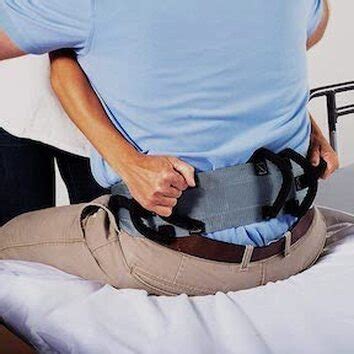
Table of Contents
While Transferring a Patient to ALS Staff: Interference Should Be Minimal
Transferring a patient to Advanced Life Support (ALS) staff requires a seamless and efficient process to ensure patient safety and optimal care. Unnecessary interference during this critical handover can compromise the quality of care and potentially endanger the patient. This article explores the crucial aspects of patient transfer to ALS, emphasizing the importance of minimizing interference and highlighting best practices for a smooth and effective transition.
Understanding the Criticality of Seamless Patient Transfers
Patient handover between medical professionals, particularly during transfers to ALS personnel, is a high-stakes situation. A smooth transfer minimizes the risk of medical errors, ensures continuity of care, and allows for the rapid implementation of advanced life support interventions if necessary. Any form of interference during this process can disrupt the established protocols, potentially leading to:
- Delayed treatment: Interference can interrupt the assessment and treatment process, delaying crucial interventions that could impact the patient's outcome.
- Medication errors: Interruptions can lead to errors in medication administration or dosage.
- Miscommunication: Distractions and interruptions can cause miscommunication of vital information, compromising patient care.
- Increased stress: A chaotic transfer environment can increase stress levels for both the transferring and receiving teams, impacting their performance.
- Patient safety concerns: The most serious consequence of interference is a compromise to patient safety. This could involve missed observations, delayed interventions, or accidental harm.
Types of Interference to Avoid During ALS Patient Transfers
Interference during patient transfer to ALS staff can manifest in various forms. Recognizing these different types is crucial for mitigating their negative impact.
1. Unnecessary Questions and Interruptions
Constant questioning or interrupting the ALS team during their initial assessment and stabilization can be highly disruptive. Allow the ALS team to conduct their assessment without interruption. Postponing questions until a suitable time will ensure a more efficient and focused handover.
2. Unsolicited Advice and Suggestions
Unless the ALS team explicitly requests assistance or guidance, refrain from offering unsolicited advice or suggestions. ALS personnel are highly trained and equipped to handle complex medical situations. Unnecessary suggestions could confuse the team and potentially impede their established protocols.
3. Physical Obstructions
Physically obstructing the ALS team's access to the patient or equipment can cause delays and hinder their ability to perform their duties effectively. Maintain a safe distance and ensure clear pathways for the ALS team to move around.
4. Unnecessary Presence of Non-Essential Personnel
The presence of excessive non-essential personnel can clutter the space, create distractions, and potentially obstruct the ALS team's workflow. Only those directly involved in the patient transfer or those essential to the patient’s immediate care should be present.
5. Disruptions to Communication
Interfering with the established communication channels between the transferring and receiving teams can lead to miscommunication of critical patient information. Allow clear, uninterrupted communication between ALS personnel and the transferring team.
6. Improper Documentation Practices
Incomplete or inaccurate documentation during the handover process can lead to misunderstandings and errors in continued patient care. Ensure proper and timely completion of all documentation, including vital signs, medication history, and treatment details. This should ideally happen before the patient is handed over.
Best Practices for Minimizing Interference During ALS Patient Transfers
Establishing clear protocols and guidelines is crucial for minimizing interference and ensuring a smooth transition.
1. Pre-Transfer Briefing
A clear and concise briefing before the transfer should outline the patient's condition, medical history, current treatment, and any potential risks or challenges. This briefing should involve only the necessary personnel.
2. Designated Roles and Responsibilities
Clearly defined roles and responsibilities for each member involved in the transfer process help maintain order and minimize confusion. One person should be designated as the main point of contact for communication.
3. Structured Handover Process
A structured handover process that follows a standardized format ensures that all critical information is relayed accurately and consistently. Tools like SBAR (Situation, Background, Assessment, Recommendation) can improve communication efficiency.
4. Clear Communication Channels
Establish clear and efficient communication channels for all involved parties, preventing unnecessary interruptions and ensuring timely information exchange.
5. Controlled Environment
Maintain a controlled environment around the patient, minimizing distractions and interruptions. This could include temporarily relocating non-essential personnel or equipment.
6. Post-Transfer Debriefing
A brief debriefing after the transfer provides an opportunity to address any issues, identify areas for improvement, and ensure a consistent approach for future transfers. This feedback loop is crucial for continuous improvement.
The Role of Training and Education in Minimizing Interference
Adequate training and education for all healthcare professionals involved in patient transfers are vital. This training should cover:
- Communication skills: Effective communication is crucial for a smooth and safe transfer. Training should focus on active listening, clear articulation, and conflict resolution.
- Teamwork and collaboration: Understanding the importance of teamwork and how to collaborate effectively with different healthcare professionals.
- Understanding ALS protocols: Knowledge of ALS protocols and procedures helps minimize unnecessary interference by understanding the team's priorities.
- Patient safety protocols: Prioritizing patient safety during all phases of the transfer process.
Legal and Ethical Considerations
Minimizing interference during patient transfer is not just a matter of efficiency but also carries significant legal and ethical implications. Failure to ensure a smooth handover can lead to negligence claims or disciplinary action. Healthcare professionals have a professional obligation to provide safe and effective care, which includes ensuring a seamless transfer process.
Conclusion: Prioritizing Patient Safety and Efficient Care
Minimizing interference during patient transfer to ALS staff is paramount for ensuring patient safety and optimal care. By following best practices, establishing clear communication channels, providing adequate training, and understanding the legal and ethical implications, healthcare professionals can improve the efficiency and safety of the patient transfer process. Every effort should be made to create a controlled, focused environment that allows the ALS team to perform their duties effectively, ensuring the best possible outcome for the patient. Remember, a successful patient transfer is a collaborative effort focused solely on the well-being of the patient.
Latest Posts
Latest Posts
-
Training Activities That Subcategorize Instructors And Students
Apr 01, 2025
-
Student Exploration Waves Gizmo Answer Key
Apr 01, 2025
-
Nursing Diagnosis For Jaundice In Newborn
Apr 01, 2025
-
Ap Calculus Bc Unit 3 Progress Check Mcq
Apr 01, 2025
-
Which Of These Is False About Lithospheric Plates
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about While Transferring A Patient To Als Staff Interference Should Be . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
