Apex Nih Stroke Scale Test Group A
Onlines
Mar 13, 2025 · 7 min read
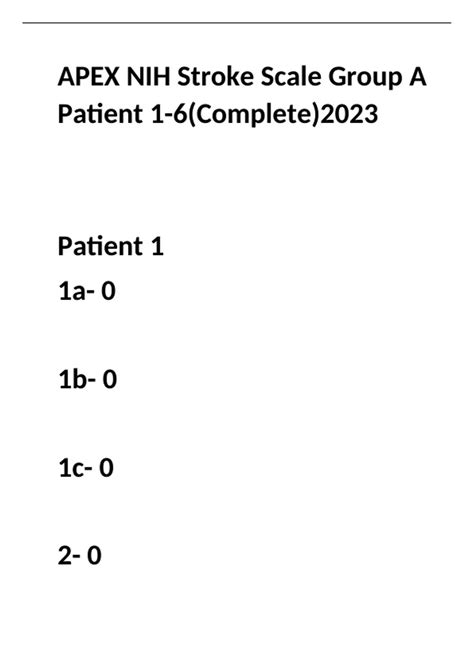
Table of Contents
Apex NIH Stroke Scale Test: Group A – A Comprehensive Guide
The National Institutes of Health Stroke Scale (NIHSS) is a standardized neurological examination used to evaluate the severity of stroke in patients. The scale is widely used globally and plays a crucial role in assessing stroke prognosis, guiding treatment decisions, and facilitating research. This comprehensive guide delves into the specifics of Group A within the Apex NIH Stroke Scale test, exploring its components, scoring, interpretation, and clinical significance. Understanding Group A is pivotal for healthcare professionals involved in stroke management.
Understanding the NIH Stroke Scale (NIHSS)
The NIHSS is composed of 11 items, each assessing a specific neurological function. Each item receives a score ranging from 0 (no deficit) to a maximum score specific to the item, with higher scores indicating more severe neurological impairment. The total score, the sum of individual item scores, ranges from 0 to 42. The higher the total score, the more severe the stroke is considered to be. The scale's structured nature ensures consistency and comparability of assessments across different healthcare settings and clinicians. The scale's utility extends beyond immediate assessment; it's vital for monitoring stroke progression and treatment response.
The scale is broadly categorized into different item groups based on the neurological function assessed. While there isn't an official "Group A" designation within the standard NIHSS documentation, this article will refer to "Group A" as a conceptual grouping of items commonly considered crucial for initial assessment and triage, focusing on the most immediately life-threatening aspects of stroke. This conceptual grouping facilitates a clearer understanding of the prioritized elements of the examination.
Group A: Prioritizing Life-Threatening Neurological Deficits
For the purpose of this article, we define “Group A” of the Apex NIH Stroke Scale as encompassing the following key components: Level of Consciousness (LOC), Gaze, Visual Fields, and Motor Function (both arms and legs). These items are crucial because they often directly indicate the presence of life-threatening complications such as brainstem involvement, respiratory compromise, and potential for rapid neurological deterioration.
1. Level of Consciousness (LOC)
The LOC assessment is paramount in evaluating a stroke patient's immediate status. This element focuses on the patient's alertness and responsiveness to stimuli. Scores range from 0 (Alert) to 4 (Stupor or Coma). A score of 3 or 4 immediately signals a severe neurological compromise requiring immediate intervention. The assessment involves observation of the patient's alertness, response to verbal stimuli, and reaction to painful stimuli. The subtleties in response, such as delayed reactions or inappropriate responses, are also carefully noted. Accurate LOC assessment provides critical insight into the patient's overall neurological status and guides immediate management decisions regarding airway, breathing, and circulation (ABCs).
Key Considerations for LOC Assessment:
- Responsiveness: The speed and appropriateness of the patient's response are crucial.
- Stimulus Type: The type of stimulus used (verbal, tactile, painful) needs to be documented.
- Documentation: Precise description of the patient's response is necessary.
- Baseline: If possible, establish a baseline LOC against previous observations.
2. Gaze
Gaze assessment determines the presence of any deviation or paralysis of eye movements. This is vital because it can indicate brainstem involvement, a serious condition often associated with significant morbidity and mortality. Scores range from 0 (Normal) to 3 (Forced deviation). A deviation of gaze, particularly if persistent and not easily correctable, suggests significant neurological damage and warrants immediate attention. The examiner assesses the patient's ability to maintain gaze in various directions, looking for any asymmetry or inability to move the eyes freely in specific directions.
Key Considerations for Gaze Assessment:
- Spontaneous eye movements: Observe the patient's resting eye position.
- Ocular motility: Test the range of eye movements in all directions.
- Symmetry: Compare eye movements between the two eyes.
- Oculocephalic reflex: In unresponsive patients, this reflex may be tested (but with caution).
3. Visual Fields
Assessing visual fields helps determine the extent of visual deficits caused by the stroke. Loss of vision in one or both visual fields can indicate damage to specific brain regions and contribute to functional limitations. Scores range from 0 (No visual loss) to 3 (Complete hemianopia). While not immediately life-threatening in the same way as brainstem involvement, significant visual field defects can impact the patient's safety and rehabilitation. The assessment typically involves confrontation testing, where the examiner compares their visual field with the patient's.
Key Considerations for Visual Field Assessment:
- Confrontation testing: A reliable and practical method for bedside assessment.
- Consistency: Compare findings between both eyes.
- Lesion localization: Visual field deficits can help localize the stroke.
- Impact on function: Note the impact of visual field defects on daily activities.
4. Motor Function (Arms and Legs)
Motor function assessment, including both arms and legs, is vital for determining the extent of motor weakness or paralysis resulting from the stroke. The assessment involves testing motor strength on a 0 to 4 scale (0 = No movement to 4 = Normal strength). This provides a quantitative measure of motor impairment, which has significant implications for functional prognosis and rehabilitation planning. Significant weakness or paralysis in one or both limbs represents a major functional deficit requiring immediate intervention and rehabilitation efforts.
Key Considerations for Motor Function Assessment:
- Muscle strength: Test strength against gravity and resistance.
- Symmetry: Compare strength between the affected and unaffected limbs.
- Drift: Observe for any pronator drift in the arms.
- Spasticity: Note any increased muscle tone or spasticity.
Interpreting Group A Scores and Clinical Significance
The combined scores from these Group A items provide a critical initial assessment of the stroke's severity. A high total score for this subset of the NIHSS strongly suggests a severe stroke with potentially life-threatening complications. This initial assessment guides immediate management decisions, including:
- Emergency Interventions: High scores may necessitate immediate interventions such as endotracheal intubation, mechanical ventilation, or intravenous thrombolysis (if eligible).
- Intensive Care Unit (ICU) Admission: Patients with high Group A scores often require close monitoring in an ICU setting.
- Neurological Monitoring: Continuous monitoring of neurological function is crucial for detecting any deterioration.
- Treatment Planning: The Group A scores inform decisions regarding appropriate treatment strategies, including rehabilitation and supportive care.
The Remaining NIHSS Components and Their Importance
While Group A provides crucial initial information, a complete NIHSS assessment is necessary for a holistic understanding of the stroke's impact. The remaining items assess: Limb Ataxia, Sensory, Language, Dysarthria, Extinction and Inattention (neglect), and others. These items contribute to a comprehensive assessment of the patient's neurological deficits and help determine the overall prognosis and guide long-term rehabilitation planning.
Limitations of the NIHSS
It's crucial to acknowledge the limitations of the NIHSS. The scale is primarily designed for acute stroke assessment and may not fully capture subtle neurological deficits or the complexity of long-term functional outcomes. Additionally, the scoring system may not equally reflect the impact of different types of strokes or individual variations in patient presentation.
Conclusion: Apex NIH Stroke Scale Test and Group A
The Apex NIH Stroke Scale Test, focusing on Group A (as conceptually defined in this article), provides a vital framework for rapidly evaluating life-threatening neurological deficits in acute stroke. While the standard NIHSS doesn’t officially utilize this grouping, understanding the critical elements of LOC, gaze, visual fields, and motor function is paramount for healthcare professionals involved in stroke management. The efficient and accurate assessment of Group A allows for timely interventions, improves patient outcomes, and facilitates effective communication and collaboration among healthcare providers. This rapid assessment should always be followed by a complete NIHSS evaluation to gain a comprehensive understanding of the stroke's impact and facilitate appropriate treatment and rehabilitation strategies. Consistent training and adherence to standardized assessment protocols are crucial for optimal utilization of the NIHSS and improving the care of stroke patients.
Latest Posts
Latest Posts
-
Mrs Ridgeway Enrolled In Original Medicare
Mar 13, 2025
-
Residents Of Griffith Park And Surrounding Neighborhoods
Mar 13, 2025
-
A Customer At A Restaurant Sees That She Was Charged
Mar 13, 2025
-
What Type Of Structure Is Shown In This Figure
Mar 13, 2025
-
Identification Of Selected Anions Lab Answers
Mar 13, 2025
Related Post
Thank you for visiting our website which covers about Apex Nih Stroke Scale Test Group A . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
