Benign Prostatic Hyperplasia Hesi Case Study
Onlines
Mar 17, 2025 · 7 min read
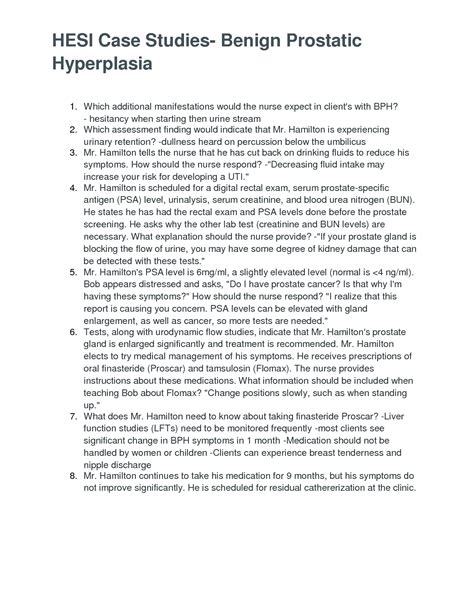
Table of Contents
Benign Prostatic Hyperplasia (BPH): A Comprehensive HESI Case Study Analysis
Benign prostatic hyperplasia (BPH), also known as an enlarged prostate, is a common condition affecting older men. This detailed HESI case study analysis will explore the multifaceted aspects of BPH, encompassing its pathophysiology, clinical manifestations, diagnostic approaches, treatment options, and nursing considerations. We'll delve into a hypothetical case study to illustrate these concepts and provide a comprehensive understanding of managing this prevalent urological condition.
Understanding Benign Prostatic Hyperplasia (BPH)
BPH is characterized by the non-cancerous enlargement of the prostate gland, leading to a range of lower urinary tract symptoms (LUTS). The exact etiology remains unclear, but hormonal changes associated with aging, particularly the imbalance between dihydrotestosterone (DHT) and estrogen, play a significant role. The increased prostate size obstructs the urethra, causing urinary symptoms.
Pathophysiology of BPH
The cellular mechanisms behind BPH involve the proliferation of prostate stromal and epithelial cells, leading to an increase in prostate volume. This growth is largely influenced by androgen receptors, particularly DHT, which stimulates cell growth and differentiation. The enlarged prostate compresses the urethra, causing obstruction and the characteristic symptoms of BPH.
Clinical Manifestations of BPH
The symptoms of BPH are highly variable, ranging from mild inconvenience to severe disability. Common LUTS include:
-
Storage symptoms: These relate to bladder filling and include urinary frequency (frequent urination), nocturia (nighttime urination), urgency (sudden, strong urge to urinate), and urge incontinence (involuntary urine leakage due to urgency).
-
Voiding symptoms: These relate to the process of urination and include hesitancy (difficulty starting urination), weak stream, intermittent stream (stopping and starting during urination), straining to urinate, and post-void dribbling (urine leakage after urination).
-
Post-micturition symptoms: These include a feeling of incomplete bladder emptying.
The severity of symptoms doesn't necessarily correlate with the prostate size. Some men with significantly enlarged prostates may experience minimal symptoms, while others with moderately enlarged prostates may suffer debilitating LUTS.
Diagnostic Evaluation of BPH
Accurate diagnosis of BPH involves a combination of patient history, physical examination, and laboratory investigations.
History and Physical Examination
A detailed history focusing on LUTS, including symptom severity and duration, is crucial. A digital rectal examination (DRE) allows the clinician to assess prostate size, consistency, and the presence of any nodules. The DRE provides a rough estimation of prostate size but isn't always accurate.
Laboratory Investigations
While BPH itself isn't diagnosed through lab tests, certain tests can be helpful in ruling out other conditions and guiding treatment decisions. These include:
- Urinalysis: To check for infection, hematuria (blood in urine), or other abnormalities.
- Blood tests: To evaluate kidney function (creatinine, blood urea nitrogen) and assess for other medical conditions.
- Prostate-specific antigen (PSA) test: While primarily used for prostate cancer screening, PSA levels can be elevated in BPH. However, an elevated PSA alone doesn't diagnose BPH.
Imaging Studies
Imaging studies aren't routinely needed for diagnosing BPH, but they might be helpful in specific cases. These include:
- Transrectal ultrasound (TRUS): Provides a more accurate assessment of prostate size and can detect any suspicious areas.
- Uroflowmetry: Measures the rate of urine flow, which helps assess the severity of urinary obstruction.
- Post-void residual (PVR) measurement: Determines the amount of urine remaining in the bladder after urination, indicating incomplete bladder emptying.
Treatment Options for BPH
Treatment approaches for BPH vary based on symptom severity and patient preference. Options range from watchful waiting to surgical intervention.
Watchful Waiting
For men with mild symptoms that don't significantly impact their quality of life, watchful waiting is a reasonable approach. This involves regular monitoring of symptoms and prostate size without immediate intervention.
Medical Management
Medical therapies aim to reduce prostate size and improve urinary flow. Common medications include:
- Alpha-blockers: Relax the muscles in the prostate and bladder neck, improving urine flow. Examples include tamsulosin, alfuzosin, and terazosin.
- 5-alpha-reductase inhibitors: Reduce DHT levels, shrinking the prostate over time. Examples include finasteride and dutasteride.
- Combination therapy: Using both alpha-blockers and 5-alpha-reductase inhibitors can provide synergistic benefits.
- Antimuscarinics: These drugs help reduce bladder spasms and urgency, primarily targeting storage symptoms. Examples include oxybutynin and tolterodine.
Minimally Invasive Procedures
For men who don't respond adequately to medical therapy or prefer less invasive options, minimally invasive procedures might be considered. These include:
- Transurethral microwave thermotherapy (TUMT): Uses heat to destroy prostate tissue.
- Transurethral needle ablation (TUNA): Uses radiofrequency energy to destroy prostate tissue.
- Laser therapy: Different laser techniques can be used to remove or shrink prostate tissue.
Surgical Intervention
Surgical intervention is considered for men with severe symptoms that don't respond to other treatments or who experience complications like urinary retention or recurrent urinary tract infections. The most common surgical procedure is:
- Transurethral resection of the prostate (TURP): Uses a resectoscope to remove excess prostate tissue. It's highly effective but carries a slightly higher risk of complications.
Nursing Considerations in BPH Management
Nursing care plays a vital role in managing BPH and improving patient outcomes. Key considerations include:
- Patient education: Educating patients about BPH, its symptoms, treatment options, and potential complications is crucial for informed decision-making and adherence to the treatment plan.
- Symptom assessment: Regularly assessing LUTS using validated tools like the International Prostate Symptom Score (IPSS) helps monitor treatment effectiveness and identify any worsening symptoms.
- Medication administration and monitoring: Nurses administer medications, monitor for side effects, and educate patients on potential drug interactions.
- Post-operative care: For patients undergoing surgical procedures, nurses provide post-operative care, including monitoring vital signs, managing pain, and preventing complications such as bleeding or infection.
- Fluid balance: Monitoring fluid intake and output is essential, especially in post-operative patients, to prevent dehydration or fluid overload.
- Promoting urinary continence: Nurses provide education and support to help patients manage incontinence, if present.
- Emotional support: BPH can significantly impact a patient's quality of life, leading to anxiety and depression. Nurses provide emotional support and encourage open communication.
Hypothetical HESI Case Study: Mr. Jones
Mr. Jones, a 72-year-old male, presents to the clinic complaining of urinary frequency, urgency, nocturia (3-4 times per night), and a weak urinary stream. He reports difficulty initiating urination and a feeling of incomplete bladder emptying. He denies hematuria or fever. His medical history includes hypertension and hyperlipidemia. On physical examination, his prostate is enlarged and firm on DRE.
1. What are the likely diagnoses?
Based on the symptoms and physical examination findings, the likely diagnosis is benign prostatic hyperplasia (BPH). Further investigations would be needed to rule out other conditions like prostate cancer.
2. What diagnostic tests would you recommend?
- Urinalysis to rule out infection or hematuria.
- Blood tests to evaluate kidney function and PSA levels.
- Uroflowmetry to assess urine flow rate.
- Post-void residual (PVR) measurement to check for incomplete bladder emptying.
3. What treatment options would you consider, and why?
Given Mr. Jones's symptoms, several treatment options could be considered:
- Watchful waiting: If his symptoms are mild and don't significantly affect his quality of life.
- Medical management: Alpha-blockers to improve urine flow could be the first-line treatment. 5-alpha-reductase inhibitors might be considered if the symptoms don't improve adequately with alpha-blockers alone or if prostate size reduction is desired.
- Minimally invasive procedures: If medical management fails or if Mr. Jones prefers less invasive options.
- Surgical intervention: As a last resort, if symptoms are severe, refractory to other treatments, or if complications arise (such as urinary retention).
4. What nursing interventions would be important for Mr. Jones?
Nursing interventions would focus on:
- Patient education about BPH, its treatment, and potential complications.
- Monitoring his symptoms using the IPSS.
- Medication administration and monitoring for side effects.
- Monitoring fluid balance.
- Providing emotional support and addressing any anxieties related to his condition.
5. What patient education would you provide?
Patient education should include information about:
- The nature of BPH and its causes.
- The importance of regular follow-up appointments.
- The expected benefits and potential side effects of the prescribed medications.
- Lifestyle modifications, such as avoiding caffeine and alcohol, which can exacerbate symptoms.
- Strategies for managing urinary incontinence, if present.
- When to seek immediate medical attention (e.g., acute urinary retention).
This comprehensive analysis of a hypothetical HESI case study on BPH demonstrates the multifaceted approach required to manage this common urological condition. Effective management necessitates a strong understanding of the pathophysiology, diagnostic methods, treatment options, and nursing implications involved in providing holistic patient care. Remember, always consult relevant medical guidelines and resources for the most up-to-date information on BPH management.
Latest Posts
Latest Posts
-
All Flags Such As Porn And Upsetting Offensive Are Query Independent
Mar 17, 2025
-
An Electrical Motor Provides 0 50 W Of Mechanical Power
Mar 17, 2025
-
Studying Marketing Should Help You To Blank
Mar 17, 2025
-
Shaping Clay On A Rapidly Turning Wheel Is Called
Mar 17, 2025
-
During The International Coronavirus Pandemic Many People
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about Benign Prostatic Hyperplasia Hesi Case Study . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
