Soap Note For Acute Otitis Media
Onlines
Mar 26, 2025 · 6 min read
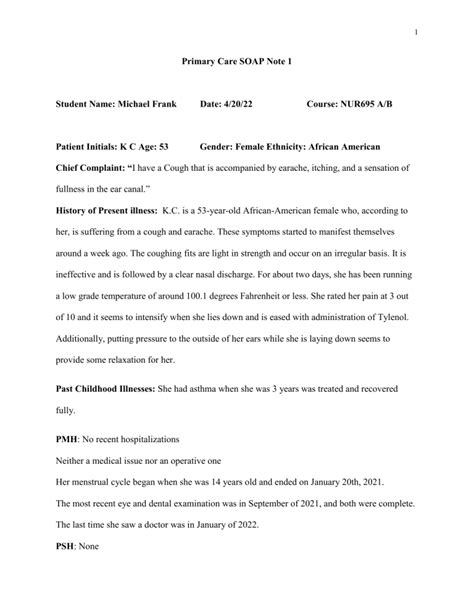
Table of Contents
SOAP Note for Acute Otitis Media: A Comprehensive Guide
Acute otitis media (AOM), or middle ear infection, is a common ailment, particularly among children. A thorough and well-structured SOAP note is crucial for accurate diagnosis, effective treatment, and seamless communication among healthcare professionals. This comprehensive guide will delve into the essential components of a SOAP note for AOM, providing examples and highlighting best practices.
Understanding the SOAP Note Format
The SOAP note framework, an acronym for Subjective, Objective, Assessment, and Plan, provides a standardized method for documenting patient encounters. Each section plays a vital role in building a complete clinical picture.
1. Subjective: The Patient's Story
This section captures the patient's perspective on their condition. For AOM, it involves detailed information gathered through patient history-taking. Key elements include:
-
Chief Complaint (CC): This concisely summarizes the patient's primary reason for seeking medical attention. Examples for AOM include: "Ear pain," "Earache," "Pulling at ear," (for infants/toddlers), "Fluid drainage from ear."
-
History of Present Illness (HPI): This expands on the CC, providing a chronological account of the symptoms. Consider using the mnemonic OPQRST to guide your questioning:
- Onset: When did the symptoms begin?
- Provoking/Palliative factors: What makes the pain better or worse? (e.g., lying down, medication, heat/cold)
- Quality: Describe the pain (e.g., sharp, dull, aching, throbbing).
- Radiation: Does the pain radiate to other areas?
- Severity: How severe is the pain on a scale of 1-10?
- Timing: How often does the pain occur? Is it constant or intermittent?
-
Past Medical History (PMH): Document any relevant past illnesses, surgeries, or hospitalizations. Include previous ear infections, allergies, and any chronic conditions.
-
Surgical History (SH): Note any previous ear surgeries, including myringotomy or tympanostomy tube placement.
-
Medications: List all current medications, including over-the-counter drugs, supplements, and herbal remedies.
-
Allergies: Specify any known allergies to medications or other substances.
-
Family History (FH): Note any family history of ear infections or hearing problems.
-
Social History (SH): This section may include information relevant to the patient's risk factors for AOM, such as daycare attendance (for children), smoking exposure (for all ages), and exposure to respiratory infections.
Example Subjective:
"7-year-old male presents with a chief complaint of right ear pain for two days. The pain is described as sharp and throbbing, worse at night, and not relieved by over-the-counter pain relievers. He denies fever, chills, or hearing loss. He attends daycare and has had one prior episode of AOM six months ago. No known allergies. Denies current medication use."
2. Objective: Measurable Findings
This section details the observable and measurable findings from the physical examination. For AOM, this includes:
-
Vital Signs: Record temperature, heart rate, respiratory rate, and blood pressure. Fever is a common finding in AOM, especially in young children.
-
Otoscopic Examination: This is the cornerstone of the objective assessment for AOM. Describe the tympanic membrane (TM) in detail, noting:
- Color: Normal (pearly gray), red, bulging
- Light Reflex: Present, absent, distorted
- Mobility: Normal, limited, absent
- Fluid level: Presence of air-fluid level
- Perforation: Presence of a TM perforation
- Discharge: Presence and character of any ear discharge (e.g., purulent, serous)
-
Other Physical Exam Findings: Note any other relevant findings, such as tenderness to palpation of the tragus or mastoid process, or signs of upper respiratory infection (URI). Inspect the nasal passages for any inflammation or drainage.
Example Objective:
"Temperature: 101.2°F (oral). Right tympanic membrane is erythematous and bulging with absent light reflex and markedly diminished mobility. Left tympanic membrane appears normal. No ear discharge noted. Mild tenderness to palpation of the right tragus. No other significant physical exam findings."
3. Assessment: Diagnosis and Rationale
This section provides the diagnosis based on the subjective and objective findings. For AOM, the diagnosis should specify:
- Type of AOM: Acute otitis media with effusion (OME) or acute suppurative otitis media (ASOM). ASOM refers to AOM with purulent discharge while OME is the presence of fluid in the middle ear without infection.
- Laterality: Specify whether the infection affects one ear (unilateral) or both ears (bilateral).
- Severity: Mild, moderate, or severe, based on the clinical presentation and severity of symptoms.
Example Assessment:
"Diagnosis: Acute suppurative otitis media, right ear, moderate severity." This diagnosis is supported by the patient's report of ear pain, fever, and the otoscopic findings of erythema, bulging TM, and absent light reflex.
4. Plan: Treatment and Follow-Up
This section outlines the treatment plan and follow-up recommendations. The plan should include:
-
Treatment: This might include:
- Analgesics: Acetaminophen or ibuprofen for pain and fever relief.
- Antibiotics: Amoxicillin is often the first-line treatment for AOM, though resistance is increasing. Consider alternatives such as amoxicillin-clavulanate, cefdinir, or azithromycin if necessary. Always consider antibiotic stewardship guidelines. For mild cases, watchful waiting may be an option.
- Decongestants: To help alleviate nasal congestion. Use with caution in children.
- Myringotomy: This is a surgical procedure to create an incision in the eardrum to relieve pressure and drain fluid. It is considered only when conservative treatment fails.
- Tympanostomy Tubes: If recurrent or severe AOM is documented, tympanostomy tubes might be recommended.
-
Patient Education: Instruct the patient and family about the disease process, medications, and when to seek immediate medical attention. Educate about pain management techniques and the importance of completing the prescribed antibiotic course.
-
Follow-up: Schedule a follow-up appointment to assess the response to treatment and monitor for complications.
Example Plan:
"1. Amoxicillin 500mg three times daily for 10 days. 2. Acetaminophen 15 mg/kg every 4-6 hours as needed for pain and fever. 3. Close observation for worsening symptoms or signs of complications. 4. Follow-up appointment in 7 days."
Addressing Specific Considerations
Several aspects need tailored attention when documenting AOM:
-
Age of the patient: Infants and young children may not be able to verbalize their symptoms, relying on parental reports and observable signs. Detailed documentation of feeding difficulties, irritability, or sleep disturbances is crucial.
-
Complications: Document any signs or symptoms suggestive of complications, such as mastoiditis, meningitis, or labyrinthitis. These require urgent attention.
-
Antibiotic Resistance: The rise of antibiotic resistance necessitates a cautious approach to antibiotic prescribing. Appropriate documentation of the rationale for antibiotic choice is crucial.
-
Watchful Waiting: In some cases of mild AOM, particularly in older children, watchful waiting may be a suitable management strategy. This should be documented explicitly, including criteria for escalating to antibiotic treatment.
-
Cultural Considerations: Be mindful of cultural beliefs and practices that may influence treatment adherence. This should be a part of patient education.
Beyond the Basic SOAP Note: Enhancing Documentation
To optimize the SOAP note for AOM and improve its value, consider these enhancements:
-
Use of standardized terminology: Employ consistent and accurate medical terminology for improved interoperability.
-
Use of objective measurements: Whenever possible, use quantifiable measurements rather than subjective descriptions (e.g., "temperature of 101.2°F" instead of "high fever").
-
Clear and concise writing: Avoid jargon and ambiguity to ensure easy comprehension.
-
Legibility: Maintain neat and legible handwriting or use electronic health records.
-
Regular review and updates: Update the SOAP note with any changes in the patient's condition or treatment plan.
By consistently implementing these guidelines, you can craft a comprehensive and effective SOAP note for acute otitis media. This enhances communication, facilitates optimal patient care, and ensures accurate medical record-keeping, benefiting both the patient and the healthcare system. Remember, a well-structured SOAP note is a cornerstone of high-quality medical care. The accuracy and completeness of your documentation not only assist in immediate treatment but can also inform future patient care decisions.
Latest Posts
Latest Posts
-
Spatial Vis Slopes And Curves Answers
Mar 29, 2025
-
Worksheet Osmosis And Tonicity Answers Key
Mar 29, 2025
-
What Mindset Helps Facilitate Unity Of Effort
Mar 29, 2025
-
Match The Windows 10 Registry Key With Its Description
Mar 29, 2025
-
Draw The Correct Product For The Given Diels Alder Reaction
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Soap Note For Acute Otitis Media . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
