Symptomatic Hypoglycemia Will Most Likely Develop If A Patient
Onlines
Mar 23, 2025 · 6 min read
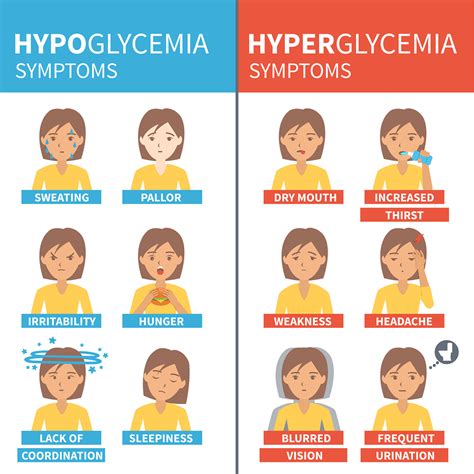
Table of Contents
Symptomatic Hypoglycemia: Understanding Risk Factors and Development
Symptomatic hypoglycemia, characterized by noticeable symptoms resulting from low blood sugar, is a serious condition that can significantly impact a patient's quality of life. Understanding the factors that predispose individuals to developing this condition is crucial for effective prevention and management. This comprehensive article delves into the various scenarios and patient profiles where symptomatic hypoglycemia is most likely to develop.
Who is at Risk for Symptomatic Hypoglycemia?
Several factors increase the risk of developing symptomatic hypoglycemia. These factors can be broadly categorized as related to:
- Diabetes Management: This is the most common cause.
- Pancreatic Conditions: Certain diseases affecting the pancreas.
- Endocrine Disorders: Issues with hormone regulation.
- Medications: Several drugs can trigger hypoglycemia.
- Dietary Habits: Extreme diets or fasting.
- Genetic Predisposition: A family history of hypoglycemia.
1. Diabetes Management and Hypoglycemia Risk
Patients with diabetes, especially those using insulin or certain oral hypoglycemic medications (like sulfonylureas), are at the highest risk for symptomatic hypoglycemia. This risk is particularly pronounced when:
- Insulin Doses are Too High: Overdosing on insulin, either accidentally or due to miscalculation, leads to a rapid drop in blood glucose. This is especially critical for those using insulin pumps or multiple daily injections.
- Delayed or Missed Meals: Skipping meals or delaying mealtimes after insulin administration prevents the body from using the available glucose, resulting in hypoglycemia.
- Increased Physical Activity: Strenuous exercise consumes glucose at a faster rate, potentially causing blood sugar to plummet, especially if insulin or oral hypoglycemic medications are taken beforehand.
- Alcohol Consumption: Alcohol can interfere with gluconeogenesis (the body's process of producing glucose) and enhance the effects of insulin, significantly increasing the risk of hypoglycemia.
- Poor Glucose Monitoring: Insufficient or inaccurate blood glucose monitoring makes it difficult to detect and correct hypoglycemia before symptoms become severe. Regular monitoring is crucial for managing insulin doses and preventing episodes.
- Kidney or Liver Disease: Impaired kidney or liver function can affect how the body processes glucose and insulin, increasing hypoglycemic risk. This is because these organs play a crucial role in glucose metabolism.
Key takeaway: Individuals with diabetes need to meticulously monitor their blood sugar levels, carefully time their meals with insulin administration, and maintain consistent physical activity levels to mitigate the risk of hypoglycemia.
2. Pancreatic Conditions and Hypoglycemia
The pancreas plays a vital role in glucose regulation. Conditions affecting the pancreas can lead to hypoglycemia. These include:
- Insulinoma: A rare tumor in the pancreas that produces excessive insulin. This leads to persistently low blood sugar, even after eating. Symptoms are often more pronounced and persistent compared to other causes.
- Pancreatitis: Inflammation of the pancreas can disrupt insulin production and glucose regulation, potentially causing hypoglycemia. This is often associated with acute episodes of pancreatitis.
- Pancreatic Cancer: In advanced stages, pancreatic cancer can significantly impact the pancreas's ability to produce necessary hormones for glucose regulation, leading to hypoglycemia.
3. Endocrine Disorders and Hypoglycemia
Several endocrine disorders can contribute to hypoglycemia. These involve hormonal imbalances that directly or indirectly affect glucose metabolism. Some of these disorders are:
- Addison's Disease: This adrenal insufficiency leads to decreased cortisol and aldosterone production, which can result in hypoglycemia.
- Hypopituitarism: Deficiency of pituitary hormones, particularly growth hormone, can impair glucose regulation.
- Glucagonoma: Although less common, glucagonoma, a tumor secreting excessive glucagon, can cause hypoglycemia in certain circumstances due to the complex interactions within the endocrine system.
4. Medications and Hypoglycemia Risk
Certain medications can increase the risk of hypoglycemia. These include:
- Sulfonylureas: These oral hypoglycemic agents stimulate insulin release from the pancreas, potentially causing hypoglycemia, especially in patients with impaired renal or hepatic function.
- Meglitinides: Similar to sulfonylureas, these medications also increase insulin secretion, carrying a similar risk of hypoglycemia.
- Salicylates (aspirin in high doses): High doses of aspirin can increase the risk of hypoglycemia by enhancing insulin's effects.
- Beta-blockers: While not directly causing hypoglycemia, beta-blockers can mask the symptoms of hypoglycemia, making it dangerous as the individual may not recognize the early warning signs. This can delay treatment and lead to more severe consequences.
5. Dietary Habits and Hypoglycemia
Extreme dietary practices can also contribute to hypoglycemia. These include:
- Prolonged Fasting or Skipping Meals: Depriving the body of glucose for extended periods leads to hypoglycemia. This is especially true for individuals with diabetes or underlying metabolic disorders.
- Very Low-Carbohydrate Diets: While these diets can be effective for weight loss, they can disrupt glucose regulation and increase the risk of hypoglycemia, especially in those with diabetes or impaired glucose tolerance.
6. Genetic Predisposition and Hypoglycemia
A family history of hypoglycemia may indicate a genetic predisposition to the condition. This doesn't directly cause hypoglycemia but may make an individual more susceptible to developing it, particularly in the presence of other risk factors.
Recognizing Symptoms of Symptomatic Hypoglycemia
Understanding the symptoms of hypoglycemia is crucial for prompt diagnosis and treatment. Symptoms can vary from person to person, but common signs include:
- Neuroglycopenic Symptoms: These are the result of the brain's decreased access to glucose. They include confusion, difficulty concentrating, dizziness, blurred vision, headache, slurred speech, drowsiness, and even seizures or coma in severe cases.
- Autonomic Symptoms: These stem from the body's attempt to raise blood sugar. Symptoms include sweating, trembling, palpitations, anxiety, hunger, and nausea.
Severity of symptoms: The severity of symptoms depends on the rate and degree of blood glucose drop. A rapid decrease is more likely to trigger noticeable symptoms than a slow decline.
When is Symptomatic Hypoglycemia Most Likely to Develop?
Symptomatic hypoglycemia is most likely to develop when a combination of risk factors is present. For instance, a diabetic patient taking insulin, skipping a meal, and engaging in intense exercise is at a considerably higher risk compared to a healthy individual. The timing is also crucial; it often occurs several hours after insulin administration or a period of fasting.
Managing and Preventing Symptomatic Hypoglycemia
Effective management and prevention strategies are essential to minimize the risk of symptomatic hypoglycemia. These strategies include:
- Regular Blood Glucose Monitoring: Frequent blood glucose checks allow for early detection and prompt intervention.
- Dietary Management: Consistent carbohydrate intake throughout the day, along with regular mealtimes, helps maintain stable blood sugar levels.
- Medication Adjustments: Working with a healthcare professional to adjust insulin doses or oral hypoglycemic medications to optimize glucose control.
- Exercise Planning: Timing exercise appropriately in relation to meals and medications is crucial to prevent hypoglycemia.
- Awareness of Symptoms: Learning to recognize the early warning signs of hypoglycemia allows for prompt treatment.
- Treatment of Underlying Conditions: Addressing any underlying medical conditions such as insulinoma or Addison's disease is vital.
- Carrying Glucose Sources: Always having readily available glucose sources (like glucose tablets or juice) helps to rapidly raise blood sugar in case of a hypoglycemic episode.
Conclusion
Symptomatic hypoglycemia is a serious condition that requires careful management and prevention strategies. Understanding the factors that increase the risk – diabetes management, pancreatic conditions, endocrine disorders, medications, dietary habits, and genetic predisposition – is critical for identifying individuals who are most vulnerable. Close collaboration with a healthcare professional is crucial for developing a personalized plan to minimize the risk of hypoglycemic episodes and maintain optimal health. Early recognition and treatment of symptoms are also vital to prevent serious complications. By implementing the recommended strategies outlined above, individuals can significantly reduce their risk and improve their overall well-being.
Latest Posts
Latest Posts
-
Creating Ld50 Graphs For Different Substances
Mar 25, 2025
-
Ftt 101 Mechanics In Firearms Quizlet
Mar 25, 2025
-
Which Of The Following Is An Example Of Subjective Information
Mar 25, 2025
-
Tina Taxpayer Makes 75000 A Year
Mar 25, 2025
-
1 5 Word Problem Practice Angle Relationships Answer Key
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about Symptomatic Hypoglycemia Will Most Likely Develop If A Patient . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
