The Fundamental Approach In Managing Denials Is
Onlines
Mar 15, 2025 · 6 min read
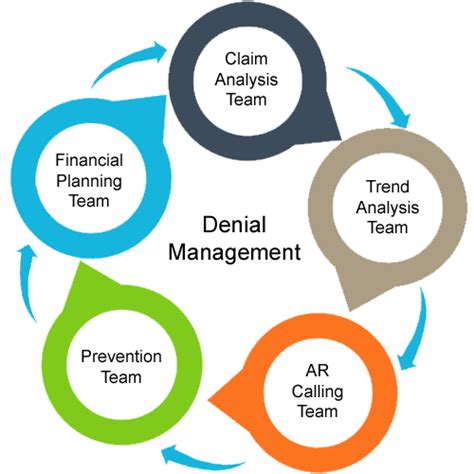
Table of Contents
The Fundamental Approach in Managing Denials: A Comprehensive Guide
Denials. The bane of any healthcare provider's existence. They represent lost revenue, increased administrative burden, and a frustrating drain on resources. Effectively managing denials isn't just about recovering lost payments; it's about building a robust, proactive system that minimizes their occurrence in the first place. This comprehensive guide delves into the fundamental approach to denial management, exploring strategies to prevent, identify, and resolve denials efficiently and effectively.
Understanding the Denial Landscape: Types and Causes
Before diving into management strategies, understanding the types and causes of denials is crucial. Denials aren't monolithic; they stem from various sources and manifest in different ways.
Common Types of Denials:
-
Medical Necessity Denials: These are arguably the most challenging. They arise when the payer determines that the services rendered weren't medically necessary for the patient's condition. This often involves rigorous documentation review and potentially requires strong appeals based on clinical evidence.
-
Coding Errors: Incorrect or incomplete coding is a leading cause of denials. This encompasses using the wrong CPT, HCPCS, or ICD codes, leading to inaccurate claims and subsequent rejection. Regular training and meticulous coding practices are paramount.
-
Eligibility Issues: Denials stemming from patient eligibility problems often occur due to outdated or incorrect information. Ensuring accurate patient demographic data and verifying eligibility prior to service delivery is vital.
-
Benefit Issues: These occur when services exceed the patient's insurance coverage or when pre-authorization wasn't obtained when required. Proactive benefit verification and adhering to payer guidelines are essential.
-
Duplicate Claims: Submitting the same claim multiple times leads to automatic rejection. Robust claim submission and tracking systems are crucial to avoid this common mistake.
-
Technical Errors: These encompass a wide array of issues, including incorrect billing addresses, missing information, or errors in the claim format. Streamlined processes and careful data entry are key.
-
Administrative Denials: These relate to procedural issues such as missing signatures or incorrect documentation submission. Clear protocols and thorough checks are needed to mitigate these.
Root Causes of Denials:
Identifying the root causes is as important as knowing the types. This involves a deeper dive into the processes and systems in place:
-
Insufficient Training: Inadequate training for coding, billing, and documentation staff can lead to numerous errors. Regular, comprehensive training programs are essential.
-
Lack of Technology: Outdated or inefficient billing software can increase the risk of errors and delays. Investing in robust, integrated systems can significantly improve accuracy and efficiency.
-
Poor Communication: Gaps in communication between clinical staff, billing staff, and payers can lead to delays and confusion. Clear, consistent communication protocols are vital.
-
Weak Internal Controls: Lack of robust internal controls, such as regular audits and quality checks, can allow errors to slip through the cracks. Implementing regular internal reviews and quality assurance programs are crucial.
-
Inadequate Documentation: Poor or incomplete medical documentation weakens the foundation of a claim, making it vulnerable to denial. Comprehensive, accurate documentation is non-negotiable.
A Proactive Approach to Denial Management: Prevention is Key
The most effective denial management strategy focuses on prevention. This involves building a robust system designed to minimize denials before they occur.
1. Pre-Service Strategies: Setting the Stage for Success
-
Patient Verification: Thoroughly verify patient insurance eligibility and benefits before services are rendered. This avoids costly denials later.
-
Pre-Authorization: Obtain necessary pre-authorization for procedures and services requiring it. This proves medical necessity and reduces the likelihood of denials.
-
Accurate Data Entry: Ensure all patient demographic and insurance information is accurate and up-to-date. This minimizes errors at the outset.
-
Clear Communication with Patients: Clearly communicate with patients about their financial responsibilities and insurance coverage. This minimizes misunderstandings and disputes.
-
Comprehensive Medical Documentation: Emphasize detailed, accurate medical documentation that supports medical necessity for all services provided.
2. During-Service Strategies: Maintaining Accuracy and Efficiency
-
Real-Time Coding: Implement systems that allow for real-time coding, improving accuracy and reducing potential errors.
-
Regular Staff Training: Provide ongoing training for coders, billers, and clinical staff on coding guidelines, billing procedures, and documentation best practices.
-
Use of Electronic Health Records (EHRs): Leverage EHR systems to streamline workflows and reduce manual data entry, minimizing potential errors.
-
Quality Control Checks: Implement rigorous internal quality control checks at various points throughout the billing process to identify and correct errors proactively.
-
Electronic Claims Submission: Utilize electronic claims submission to reduce processing time and minimize manual errors.
3. Post-Service Strategies: Addressing and Resolving Denials
Even with proactive measures, some denials are inevitable. A robust post-service strategy is crucial to address and resolve them efficiently.
-
Prompt Denial Identification: Establish a system for timely identification of denials, ensuring they aren't overlooked.
-
Categorization and Analysis: Categorize denials to identify trends and patterns, enabling targeted interventions to prevent recurring issues.
-
Efficient Appeals Process: Develop a streamlined appeals process with clear guidelines and dedicated personnel to manage the appeals process effectively.
-
Tracking and Monitoring: Closely track denial trends and resolution rates to monitor the effectiveness of implemented strategies.
-
Data-Driven Decision Making: Use data analytics to identify areas for improvement and refine denial management processes continuously.
Technological Advancements in Denial Management
Technology plays a crucial role in modern denial management. Several tools and systems can significantly improve efficiency and accuracy.
-
Denial Management Software: This specialized software automates many aspects of the denial management process, including identification, categorization, analysis, and appeals.
-
Automated Claims Scrubbing: Automated systems can identify and flag potential coding and billing errors before claims are submitted, preventing many denials proactively.
-
AI-Powered Solutions: Artificial intelligence is increasingly used to analyze denial patterns, predict potential issues, and automate the appeals process.
-
Reporting and Analytics Dashboards: Sophisticated dashboards provide real-time visibility into denial rates, trends, and resolution times, allowing for data-driven decision-making.
The Human Element: Training and Collaboration
While technology is invaluable, the human element remains crucial. A successful denial management strategy requires:
-
Well-Trained Staff: Invest in comprehensive training for all staff involved in the revenue cycle, including coders, billers, and clinical staff.
-
Collaboration and Communication: Foster strong collaboration and communication between different departments, including clinical, billing, and coding teams.
-
Dedicated Denial Management Team: Consider establishing a dedicated denial management team to focus solely on identifying, analyzing, and resolving denials.
-
Continuous Improvement: Regularly review and refine denial management processes based on data analysis and feedback from staff.
Conclusion: Building a Resilient System
Effective denial management is a continuous process, not a one-time fix. By adopting a proactive, multi-faceted approach that emphasizes prevention, efficient processes, technological advancements, and skilled personnel, healthcare providers can significantly reduce denials, improve revenue cycle performance, and ultimately, enhance patient care. Remember, the fundamental approach is built on prevention, efficient processes, and a commitment to continuous improvement. By focusing on these core tenets, you can build a resilient system that minimizes the impact of denials and strengthens your financial health.
Latest Posts
Latest Posts
-
Participant Motivation Is Usually The Result Of
Mar 17, 2025
-
All Flags Such As Porn And Upsetting Offensive Are Query Independent
Mar 17, 2025
-
An Electrical Motor Provides 0 50 W Of Mechanical Power
Mar 17, 2025
-
Studying Marketing Should Help You To Blank
Mar 17, 2025
-
Shaping Clay On A Rapidly Turning Wheel Is Called
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about The Fundamental Approach In Managing Denials Is . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
